Filing for disability benefits with the VA for a mental health condition can feel overwhelming. You know your military service changed you, leaving scars you can’t always see. But getting the VA to understand that connection often feels like an uphill battle for your VA claim.
This guide explores Mental Health Claims and the VA: How to Prove Service Connection with Medical Evidence. Many veterans suffer through this claims process. It’s tough proving something invisible, especially years after leaving the service, and veterans face unique challenges gathering evidence.
You’re not alone if you feel frustrated or lost when trying to establish service connection. Understanding how to effectively present your case for disability compensation is crucial. We’ll discuss the types of medical evidence, including treatment records and personal statements, that strengthen your VA disability claim.

Understanding the Challenge: Why VA Mental Health Claims Are Tough
Mental health conditions like post-traumatic stress disorder (PTSD), anxiety, depression, or issues related to Military Sexual Trauma (MST) carry specific hurdles in the VA system. For one, there’s still a stigma surrounding mental health conditions, both in society and sometimes within the military culture itself. This can make it hard for service members to talk about or even acknowledge the struggles they experienced.
Unlike physical injuries sustained during service, the impact mental health conditions have aren’t always immediately obvious. Symptoms might develop slowly over time, or you might have tried to push through them for years. This delay can make connecting the health condition back to your time in service seem harder, making it difficult to prove service connection.
The VA also has specific rules about what qualifies as medical evidence for disability claims. They need more than just your word; they look for documented proof in service treatment records or other medical records. Remembering specific dates, events, or symptoms from years ago can be incredibly difficult, particularly when dealing with trauma’s effects on memory.
The Core of Your Claim: Establishing Service Connection
To win any VA disability claim, including one for mental health, you generally need to establish service connection. This involves proving three key elements. Think of these as the essential supports for your claim va makes decisions on.
First, you need a current diagnosis of a mental health condition. This diagnosis must come from a qualified healthcare professional, like a psychiatrist or psychologist. Simply feeling anxious or depressed isn’t enough; you need an official diagnosis such as Major Depressive Disorder, Generalized Anxiety Disorder, or post-traumatic stress disorder.
Second, you need medical evidence or lay evidence of an event, injury, or illness that occurred during your military service. For mental health, this could be a specific traumatic event (like combat trauma or combat-related stress), a period of high stress, experiences related to MST, or even exposure situations like those involving Agent Orange for Vietnam veterans or specific concerns for Gulf War veterans. It’s the proof that something relevant happened during your va service.
Third, and often the most critical part for a successful connection claim, is the medical nexus. This is the link connecting your current diagnosis directly back to that in-service event, injury, or stressor. A medical professional needs to state that it is “at least as likely as not” (a 50% or greater probability) that your military service caused or aggravated your current condition.
This “at least as likely as not” standard means the evidence supporting connection is equal to or outweighs the evidence against it. The VA explains its evidence needs here. Without this medical evidence linking the condition to service, the VA is likely to deny the claim.
Medical Evidence That Makes a Difference for Mental Health Claims and the VA: How to Prove Service Connection with Medical Evidence
Simply having service records and attending a VA Compensation & Pension (C&P) exam often isn’t enough to build a strong mental health disability claim. The right medical evidence is what truly strengthens your case for va disability benefits. This evidence needs to clearly show the current diagnosis, the evidence linking it to service, and the severity of your symptoms and their impact on your daily life.

Your Own Medical Records (Service and Private)
Gathering all your relevant medical records is a fundamental first step in gathering evidence. This includes your Service Treatment Records (STRs). Look carefully within your service treatment records for any mention of stress, anxiety, sleep problems, visits to mental health clinics, behavioral flags, or even physical symptoms like headaches or stomach issues that can sometimes accompany mental distress.
Obtaining your STRs might require requesting them from the National Archives if you’ve been out for a while, or through the VA itself. Don’t forget about private medical records from after you left service. If you saw a civilian doctor, therapist, or counselor for your mental health condition, these treatment records are vital for your VA disability claim.
These post-service records show continuity of symptoms and treatment, painting a clearer picture of your ongoing struggles since your military service ended. They demonstrate that the condition began or worsened due to service and has persisted. Consistent treatment records can significantly bolster your claim.
Buddy Statements and Lay Evidence
Evidence doesn’t always have to come from doctors or healthcare professionals. Statements from people who knew you before, during, and after service can be powerful components of your va claims evidence. These are often called ‘buddy statements’ or, more broadly, lay statements.
Friends, family members, spouses, clergy, coworkers, or fellow service members can write about the changes they observed in your personality, behavior, or mood. Did you become more withdrawn, irritable, or anxious after a deployment or specific in-service event? Did you start having trouble sleeping, concentrating, maintaining relationships, or performing at work?
These personal statements help corroborate your own reports and can fill gaps where medical evidence might be thin or non-existent, especially if you didn’t seek formal service treatment during your military service. They should describe specific observations and changes, focusing on the impact on your daily life. The VA recognizes the value of lay statements when adjudicating disability claims.
Independent Psychological Evaluations (IPEs)
An Independent Psychological Evaluation, sometimes called an Independent Medical Opinion (IMO) when done by a psychologist or psychiatrist, can be incredibly beneficial for your va disability claim. This is an evaluation performed by a private medical professional, not one contracted by the VA for a C&P exam.
These independent evaluators often spend much more time with you than a C&P examiner might, allowing for a deeper understanding of your history and current condition. They conduct a thorough review of your records (including STRs and private treatment records), listen carefully to your history, and perform relevant psychological testing. Crucially, they understand the specific language and criteria the VA uses for assigning a disability rating.
An IPE provides a detailed assessment of your mental health condition, its severity, and its functional impact. Most importantly, it offers a professional opinion on its connection to your military service – the vital nexus. This independent viewpoint can carry significant weight, especially if a VA C&P exam was brief, unfavorable, or seemed to downplay your symptoms.
Nexus Letters: Connecting the Dots
A Nexus Letter is a specific type of medical opinion written by a qualified healthcare provider. Its sole purpose is to establish that crucial link – the nexus – between your current mental health condition and your military service experience or a specific in-service event.
A strong Nexus Letter clearly states the likelihood connection, typically using the “at least as likely as not” standard required by the VA. The provider explains their rationale thoroughly, referencing specific evidence from your service records, private treatment notes, lay statements, and their own evaluation or examination findings. It explicitly connects the dots for the VA reviewer, leaving little room for doubt about the service connection claim.
The credibility of the healthcare professional writing the letter matters significantly. A letter from a psychologist or psychiatrist who specializes in veteran evaluations and understands VA processes is generally more persuasive. They know how to articulate the medical evidence linking your condition to service in terms the VA understands, strengthening your case for disability benefits.

Detailed Medical Record Reviews
Sometimes, your medical history is extensive and complex, spanning military service and years of civilian treatment. A detailed Medical Record Review involves an expert, often a clinician or someone trained in medical analysis, carefully combing through all these documents. They synthesize the information, identify key pieces of evidence supporting your claim, and present it in a clear, organized manner.
This review can highlight patterns of symptoms, treatment responses, relevant events (like combat trauma or other stressors), and diagnoses that might otherwise get lost in a thick file. It essentially creates a roadmap of your medical history for the VA, making it easier for them to see the progression and establish service connection for your health condition. Think of it as organizing the puzzle pieces so the final picture is obvious for the claims adjudicator.
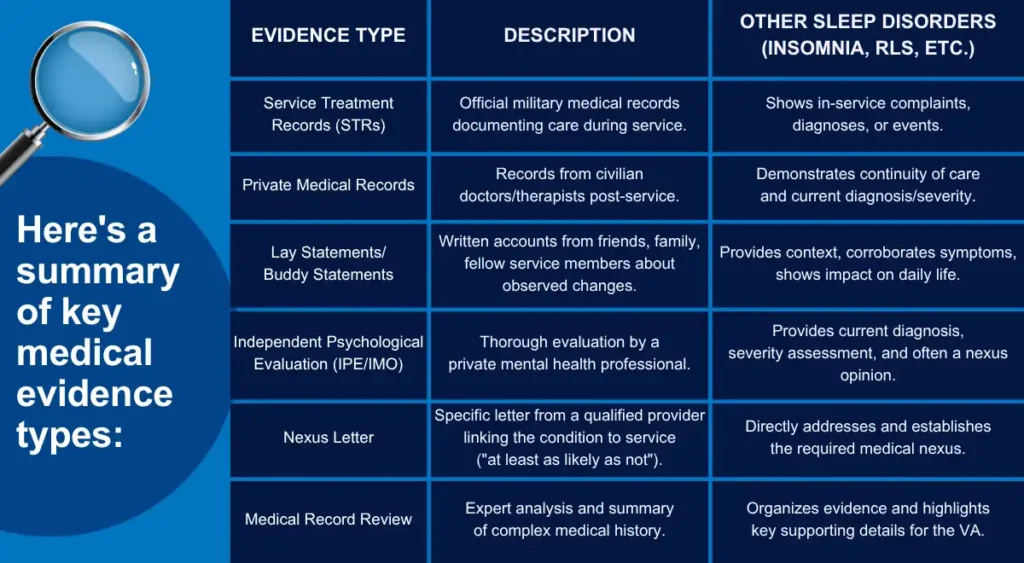
Here’s a summary of key medical evidence types:
The C&P Exam: Necessary, But Often Not Enough
As part of the claims process, the VA will likely schedule you for a Compensation and Pension (C&P) exam for your mental health condition. Attending this exam is mandatory; failing to attend can result in denial of your disability claim. A VA-contracted examiner (like a psychologist or psychiatrist) will interview you, review your file (often briefly), and provide an opinion to the VA regarding diagnosis, nexus, and severity.
However, these exams often have limitations that veterans should be aware of. They can be quite short, sometimes lasting less than an hour, which may not be sufficient to fully explore a complex history of trauma or mental health struggles. The examiner may not have deep expertise in your specific type of trauma or condition, whether it’s related to combat-related stress, MST, or other service experiences.
Some veterans report feeling rushed, misunderstood, or that the examiner seemed to minimize their symptoms or the impact on their daily life. Because the C&P examiner works for the VA (either directly or as a contractor), their opinion might sometimes feel less objective than an independent evaluation secured by the veteran. Relying solely on the outcome of the C&P exam can be risky for your VA disability claim.
If the C&P exam results are unfavorable or don’t fully capture the extent of your disability, it can significantly harm your claim for disability compensation. This is why having your own strong, independent medical evidence, like an IPE or Nexus Letter, is so important. It provides a counterbalance, offers a more complete picture of your situation, and can be crucial if you need to pursue veterans’ claim.
Understanding VA Disability Ratings for Mental Health
Once service connection is established for a mental health condition, the VA assigns a disability rating. This rating, expressed as a percentage (0%, 10%, 30%, 50%, 70%, or 100%), determines the amount of monthly disability compensation you receive. The VA uses the General Rating Formula for Mental Disorders (38 CFR § 4.130) to evaluate the level of occupational and social impairment.
The ratings range reflects the severity of symptoms and their impact on your ability to function. A 0% rating means a condition is service-connected but doesn’t currently cause significant impairment, while a 100% rating indicates total occupational and social impairment. Ratings like 30%, 50%, and 70% reflect varying degrees of difficulty in work and social settings.
It’s important to provide evidence detailing how your symptoms affect your work, relationships, self-care, and overall daily life. Lay statements from family members and your own personal statements can be very helpful here. The goal is to paint a clear picture for the VA rater of the functional limitations caused by your service-connected mental health condition, ensuring the assigned disability rating accurately reflects your level of impairment.
Special Considerations: PTSD, Anxiety, Depression, MST
While the general principles apply to all mental health claims, some conditions have specific nuances. For PTSD related to combat, the VA may concede the stressor (the traumatic event) if you served in a certain location or conflict recognized for combat exposure. You still need a current diagnosis and medical evidence linking the PTSD to that stressor.
For non-combat PTSD or PTSD from other events (like training accidents, assaults, or MST), you often need credible supporting evidence that the stressful event occurred during your military service. This might come from service records, military police reports, or lay statements from fellow service members who witnessed or knew about the event. The National Center for PTSD provides extensive resources.
Military Sexual Trauma (MST) claims also require sensitivity and specific types of evidence, as the VA understands that MST often goes unreported. They look for ‘markers,’ which are signs, events, or circumstances noted in records or reported by others that provide indirect evidence the traumatic event likely occurred. Examples include documented changes in work performance, substance abuse issues arising in service, requests for transfers, visits to medical for vague physical complaints without clear cause, or unexplained behavioral changes noted in service records or reported by buddies or family members.
For anxiety and depression, the key remains demonstrating the condition began or worsened significantly due to military service. Showing a pattern of symptoms beginning during or shortly after service through service treatment records, private medical records, and lay statements is vital. Sometimes these conditions develop secondary to service-connected physical injuries, which is another avenue for establishing service connection (secondary conditions).

Taking Control: Being Proactive with Your Evidence
Don’t wait for the VA to build your case for you when filing a disability claim. The most successful VA claims are often those where the veteran takes a proactive approach to gathering evidence. Start gathering your medical records (both service treatment records and private records) and reaching out to potential sources for buddy statements or personal statements as early as possible in the claims process.
Consider obtaining independent medical evidence, such as an IPE or a strong Nexus Letter, before you even file your claim, or early in the process after filing. Working with professionals who specialize in VA mental health claims can make a huge difference. Organizations and accredited VA representatives familiar with VA requirements can help develop the kind of robust medical evidence that clearly articulates service connection.
Finding qualified professionals is important. Look for psychologists or psychiatrists experienced with veteran evaluations and the specific criteria the VA uses. That said, many veterans have found success by actively managing their claim with the right support team. That’s where Vet Claim Solutions comes in — we connect you with experienced professionals who understand what it takes to build a strong VA disability claim.
Think of it as investing in the foundation of your claim. Strong, clear, independent medical evidence provides the best possible chance for a successful outcome and receiving the va disability benefits you earned. If your initial claim is denied, this evidence becomes even more critical for pursuing options like a higher-level review or filing a supplemental claim with new and relevant evidence.
Conclusion
Handling the VA claims process for a mental health condition can feel isolating, but you absolutely don’t have to go through it alone. Understanding the importance of robust medical evidence is your most powerful tool to prove service connection. Establishing this link often requires more than just service records and attending a C&P exam; it demands clear, expert opinions and supporting documentation that bridge the gap between your time in the military and your current diagnosis.
Remember, seeking help with Mental Health Claims Medical Evidence is a sign of strength, not weakness. Gathering independent psychological evaluations, strong nexus letters, lay statements from family members or fellow service members, and detailed medical record reviews can significantly strengthen your VA disability claim. This proactive approach improves your chances of getting the disability benefits you earned through your dedicated military service.
Don’t be discouraged if the process seems long or if you face setbacks like an claim denied decision. Persistence and strong medical evidence linking your current condition to your service are key. By understanding the requirements and actively participating in gathering evidence, you take control of your claim and move closer to securing the support you deserve.

