Insomnia affects thousands of veterans, often tied to PTSD, pain, or medications. See how medical nexus letters can establish your service connection.
Insomnia isn’t just “normal veteran stuff” — for many veterans, chronic sleeplessness has real medical and functional consequences. While the VA does not typically list “insomnia” as a separate disability, insomnia can still qualify for VA disability benefits, especially when it’s linked to service-connected conditions like PTSD, chronic pain, or medications. Understanding how the VA evaluates sleep disorders, and gathering the right medical evidence, can make the difference in your claim.
At Attain Med Group, we specialize in helping veterans build strong, medically sound claim packages — including nexus letters, medical record reviews, and DBQs — so that your insomnia can be properly documented, connected to service, and rated fairly.

In this guide, you’ll learn:
- How the VA views insomnia in its rating system
- The types of service connection that apply to insomnia
- The evidence you need — diagnosis, nexus, and functional impact
- Practical tips for your C&P exam
- Common pitfalls — and how Attain Med Group helps you avoid them
1. How the VA Treats Insomnia in Disability Claims
Insomnia Often Rated as a Symptom, Not a Standalone Diagnosis
- The VA does not have a separate diagnostic code (DC) for insomnia. Instead, insomnia is most often rated under the General Rating Formula for Mental Disorders (38 C.F.R. § 4.130).
- Because of this, insomnia is frequently evaluated as part of another service‑connected mental health condition, such as PTSD, anxiety, or depression.
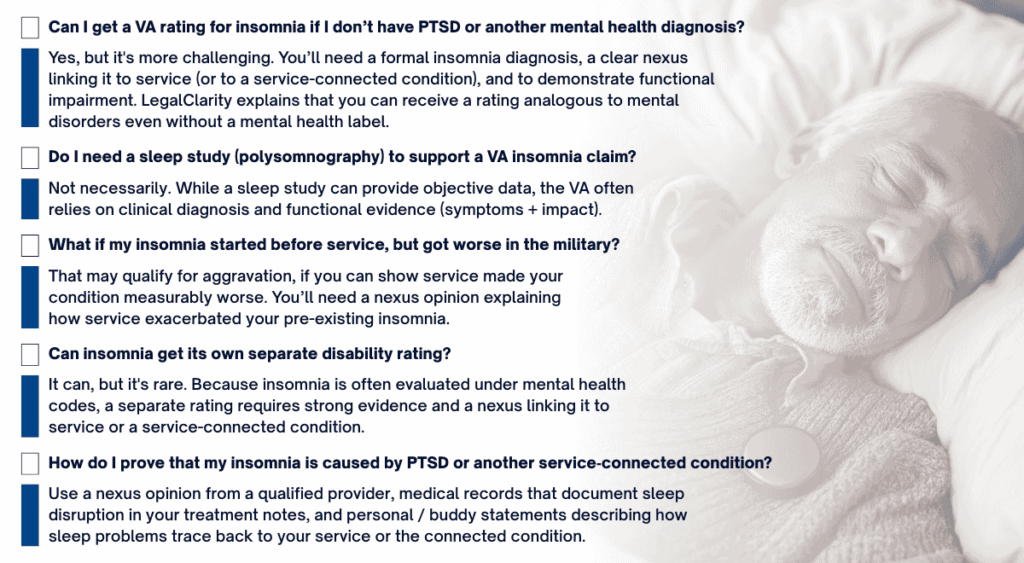
- According to VA Claims Insider, if insomnia is caused by a different service-connected physical condition (like pain) or another primary disability, a separate rating may be possible — but only with strong medical nexus evidence.
- Veterans Law Group likewise notes that VA requires a formal diagnosis (not just “poor sleep”) and a demonstrated connection to service.
What the VA Looks for in Rating Insomnia
Because insomnia is rated under the mental disorders schedule, the VA considers:
- Frequency and duration of sleep difficulties (difficulty falling asleep, staying asleep, early awakenings)
- Daytime impairment: fatigue, mood, cognition, concentration, memory, social and occupational functioning
- The VA/DoD clinical practice guideline for insomnia defines criteria similar to DSM or ICSD (International Classification of Sleep Disorders): sleep problems at least 3 nights/week for at least 3 months, despite adequate opportunity to sleep.
- Whether other sleep disorders or medical/mental health conditions better explain the insomnia symptoms.

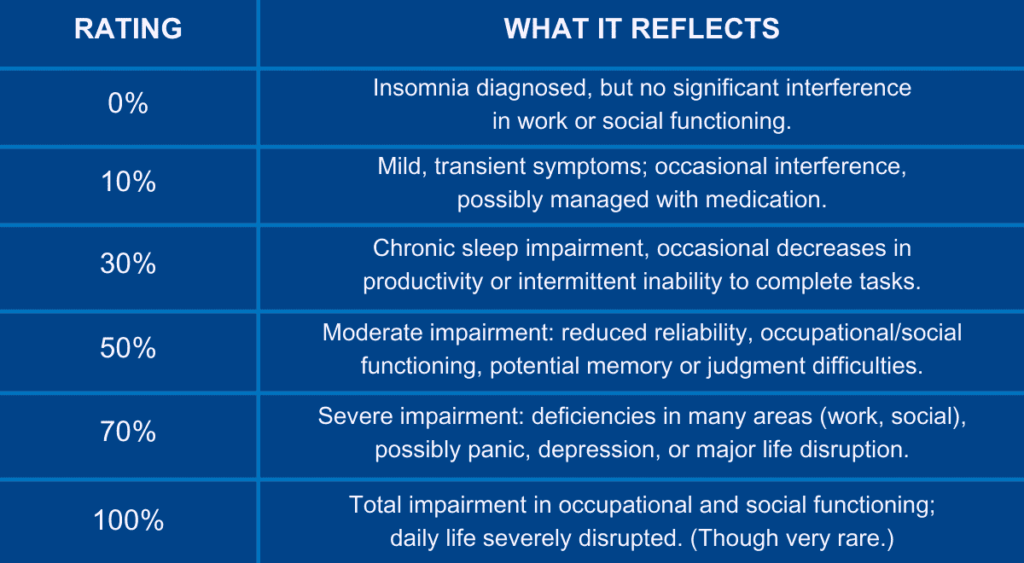
VA Disability Rating Ranges for Insomnia Symptoms
VeteransGuide and LegalClarity provide insight into how VA may rate insomnia-like symptoms:
2. Ways to Establish Service Connection for Insomnia
To get VA disability for insomnia, you must show service connection. Here are the main pathways:
A. Direct Service Connection
- Insomnia began during active service (or soon after), and there are service treatment records (STRs) documenting sleep problems or early diagnoses.
- A nexus letter from a medical provider (psychiatrist, sleep specialist) that strongly links your insomnia to service, using “at least as likely as not” medical probability language.
B. Secondary (or “Secondary to”) Service Connection
- Insomnia developed because of another service-connected condition, such as PTSD, chronic pain, or TBI.
- A medical opinion (nexus) is critical: a qualified physician must explain how the primary service-connected condition caused or aggravated your insomnia.
- Treatment records, mental health notes, and sleep logs help show the timeline and severity.
C. Aggravation
- If you had insomnia (or sleep issues) before service, but military service worsened it, you may be able to claim aggravation. LegalClarity notes that a nexus opinion must show how service made the condition worse.
3. What Evidence You Need to Build a Strong Insomnia Claim
Gathering the right evidence is crucial — especially because insomnia is inherently subjective. Here’s a breakdown:
A. Clinical / Medical Evidence
- Formal Diagnosis
- Diagnosis documented by a qualified provider (psychiatrist, psychologist, or sleep specialist).
- Use of accepted diagnostic criteria (DSM‑5, ICSD-3, or VA clinical guideline criteria). VA/DoD guidelines define “chronic insomnia disorder” as problems at least 3 nights/week for ≥3 months.
- Diagnosis documented by a qualified provider (psychiatrist, psychologist, or sleep specialist).
- Treatment Records
- Mental health notes documenting sleep complaints (VA and non-VA).
- Records of sleep medications (e.g., trazodone, zolpidem), therapy, or behavioral interventions.
- Sleep study (polysomnography) if done, though not always required for insomnia. LegalClarity notes it’s more about diagnosis + functional impact than mandatory sleep study.
- Mental health notes documenting sleep complaints (VA and non-VA).
- Independent Medical Opinion / Nexus Letter
- A physician’s letter that links your insomnia to service (direct), or to a service-connected condition (secondary).
- The opinion should explain: diagnosis, onset, progression, medical reasoning, and the causal pathway (for example, “PTSD hyperarousal causes difficulty initiating sleep”). VetNexusMD emphasizes the importance of a nexus opinion from a specialist to clearly articulate “at least as likely as not” connection.
- A physician’s letter that links your insomnia to service (direct), or to a service-connected condition (secondary).
B. Functional / Lay Evidence
- Sleep Diary / Log
- Track bedtime, wake time, awakenings, sleep duration, quality, medications, naps, daytime fatigue, and how you feel.
- Track bedtime, wake time, awakenings, sleep duration, quality, medications, naps, daytime fatigue, and how you feel.
- Personal Statement
- Use VA Form 21-4138 (“Statement in Support of Claim”) to describe how insomnia affects your daily life: concentration, mood, work, relationships.
- Use VA Form 21-4138 (“Statement in Support of Claim”) to describe how insomnia affects your daily life: concentration, mood, work, relationships.
- Buddy Statements (“Lay Statements”)
- Letters from family, friends, or fellow service members who have observed how your lack of sleep affects your functioning.
- Letters from family, friends, or fellow service members who have observed how your lack of sleep affects your functioning.
C. C&P Exam Preparation
- Bring your sleep diary, buddy statements, and medical records.
- Clearly describe your symptoms: how often you struggle to fall asleep, how many times per night you wake, how long it takes to fall back asleep, morning fatigue.
- Explain how insomnia affects your life outside the exam — not just on “bad nights.”
4. Common Challenges & How to Overcome Them
Here are several challenges veterans often face in insomnia claims — and strategies to address them:
- No Separate Diagnostic Code
- Because insomnia is often rated under mental health, it may be “lumped in” with another disorder. But a well-supported nexus opinion can help justify a distinct sleep-focused rating.
- Because insomnia is often rated under mental health, it may be “lumped in” with another disorder. But a well-supported nexus opinion can help justify a distinct sleep-focused rating.
- Lack of Formal Diagnosis
- If your medical records don’t include “insomnia disorder,” ask your provider (VA or civilian) to formally diagnose it, referencing VA/DoD guidelines.
- If your medical records don’t include “insomnia disorder,” ask your provider (VA or civilian) to formally diagnose it, referencing VA/DoD guidelines.
- Subjective Nature of Symptoms
- Use objective tools: a sleep diary, logs, functional impact statements, and third-party observations to provide the detail VA examiners need.
- Use objective tools: a sleep diary, logs, functional impact statements, and third-party observations to provide the detail VA examiners need.
- Appeals or Denials
- If denied, you may need to submit additional nexus evidence or clarify the link between your sleep issues and service. A medical opinion emphasizing causation or aggravation can be powerful in appeals.
- If denied, you may need to submit additional nexus evidence or clarify the link between your sleep issues and service. A medical opinion emphasizing causation or aggravation can be powerful in appeals.
- Pyramiding Rules
- Under 38 C.F.R. § 4.14 (pyramiding), you cannot claim separate ratings for overlapping symptomatology. That means if your insomnia overlaps heavily with a mental condition you’re already rated for, the VA may combine those rather than give separate ratings.
- Under 38 C.F.R. § 4.14 (pyramiding), you cannot claim separate ratings for overlapping symptomatology. That means if your insomnia overlaps heavily with a mental condition you’re already rated for, the VA may combine those rather than give separate ratings.
6. Why Expert Medical Opinions from Attain Med Group Are Critical
When it comes to insomnia claims, the nexus letter is often the linchpin — it’s what ties the medical facts to the legal standard. Here’s how Attain Med Group helps veterans get this right:
- Veteran‑Owned Experience + Empathy
We understand how sleep issues affect veterans’ quality of life and how they intersect with service-related trauma. - Qualified Clinicians
Our network includes psychiatrists, psychologists, and sleep specialists who know VA criteria and can provide strong, reasoned nexus letters. - Full Record Review
We examine your service treatment records, C&P exams, VA and non-VA medical files, and your own sleep diary/logs to craft a comprehensive medical narrative. - DBQ Support
We can assist your treating provider in completing a mental health DBQ or sleep disorder–relevant DBQ that clearly captures severity, frequency, and functional impact. - Strategic Submission & Appeals
Whether you are filing a new claim or appealing a denial, we help package your evidence so it addresses VA’s concerns and maximizes your chance of a favorable outcome.

Conclusion & Call to Action
Yes — you can get a VA rating for insomnia, but it requires more than just “I can’t sleep.” You need a formal diagnosis, a strong nexus linking it to your service (or a service-connected condition), and clear documentation of how your sleep problems impair your daily life.
At Attain Med Group, we’ve helped veterans just like you secure fair VA compensation by building evidence-backed, expert-supported claims. If you’re ready to get serious about your insomnia claim — or need help strengthening an appeal — we’re here for you.
→ Contact us today to schedule a free consultation
→ Download our Insomnia Claim Checklist to get started on gathering the right evidence