If you are a veteran, you likely know the VA is not great at telling you the full story about your VA disability benefits. You might have a few service connected ratings, but you still feel worse physically and mentally than what your current combined rating shows on paper.
This is where most common secondary conditions veterans miss. How to medically connect them really starts to matter. We are talking about the hidden issues that creep in years after your discharge. These are problems that quietly grow from the conditions you already have connected.
Most vets are shocked when they find out how many health issues can be claimed as a secondary service connection. The truth is, the VA rating system covers conditions that are caused or made worse by a service-connected disability. You just have to know how to show the link, and that is what you are going to see here as we walk through Most common secondary conditions veterans miss. How to medically connect them step by step.

What “Secondary Service Connection” Really Means For You
Let’s strip out the legal noise for a minute. A secondary condition is a disability that exists because of another disability the VA already recognizes as service connected. This concept is vital for increasing your overall disability rating.
Under 38 CFR 3.310(a) and (b), VA can grant service connection when a condition is directly caused by, or aggravated by, an existing service-connected condition. The regulation is also explained again at 38 CFR § 3.310 Disabilities that are proximately due to, or aggravated by, service-connected disease or injury.
That “caused by or aggravated by” line is the key phrase. You are trying to prove one of two things for your secondary service-connected claim. Either your first condition caused a new one, or it clearly made it worse over time.
Many veterans focus only on their primary service-connected issues. However, ignoring the secondary issues leaves potential compensation unclaimed. Understanding the definition of a secondary service-connected disability can change the trajectory of your medical care and financial support.
Why Veterans Miss So Many Secondary Conditions
If you feel like you have been underpaid for years, you are not alone. There are a few common reasons vets miss these important service-connected conditions.
First, most of us grew up in a “suck it up” culture during our military service. We might get knee pain rated, but we never mention the low back pain that showed up from limping for years. This mindset leads many to ignore a valid medical condition until it becomes severe.
Second, no one at the VA sits down and explains your options regarding VA benefits. You have to go digging on your own,
Third, symptoms pop up slowly. You may not realize your sleep apnea is related to your PTSD. You might not know your heart problems came from long term hypertension, which itself came on during your service years.
Finally, the confusion around medical conditions often prevents action. Veterans assume a new ailment is just aging. They do not realize it is one of many service-connected disabilities evolving from an original injury.

How The VA Looks At Medical Evidence For Secondary Claims
Before we talk about the most common secondary conditions veterans miss. How to medically connect them in real life, you need to see how the VA thinks. When reviewing a va claim, raters look for three main parts.
- A current diagnosed secondary condition.
- An already service connected primary disability.
- A medical opinion linking the two, using “at least as likely as not” language.
The legal standard is not “beyond a shadow of a doubt.” It is a 50–50 standard. If the medical documentation shows it is at least as likely as not that the primary condition caused or aggravated the secondary one, you should win that piece of the claim under 38 CFR § 3.310.
This is where a strong nexus letter becomes essential. This document connects the dots between your service and your current health. Without this link from a healthcare provider, your claim may struggle.
Strong evidence usually comes from medical literature, like research in PubMed, combined with a doctor’s written opinion. When you file VA claims, having this scientific backing helps the rater understand the progression of your disability.
Most Common Secondary Conditions Veterans Miss. How to Medically Connect Them
You have probably seen posts online listing the most common secondary service-connected disabilities. A good starting point is the coverage shown in the article shared across multiple outlets about top 5 secondary service connected disabilities and how to claim them.
Those posts are helpful, but they rarely sit next to you and say “Here is how you prove this for your life.” We will break down the secondary conditions that show up again and again for veterans. We will also show how you can medically link them in a clear, repeatable way.
The table below outlines some frequent connections to help you brainstorm.
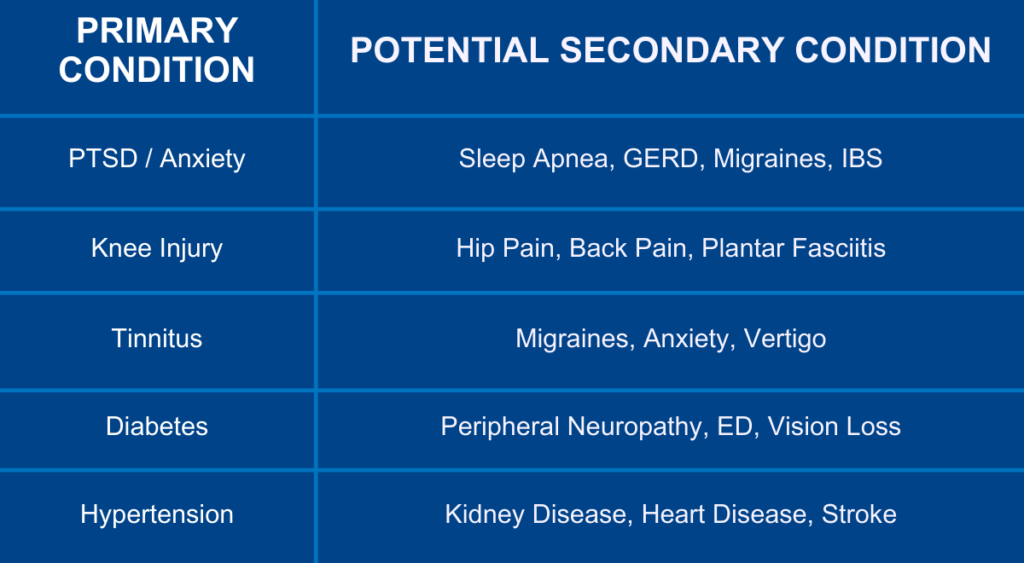
Understanding these pairings is the first step. Next, we will examine specific categories to help you build your service-connected disabilities list effectively.
1. Mental Health Conditions And Their Secondary Chains
Mental health is one of the biggest “silent drivers” of secondaries. The VA rates PTSD, depression, and anxiety using the General Rating Formula for Mental Disorders under 38 CFR § 4.130. A stress disorder rating can be the foundation for many other claims.
Once you have a rating there, a whole tree of secondary problems often grows from that single trunk. These are not in your head. They are documented in medical literature and in VA rating schedules.
If you also suffered a traumatic brain injury, the overlap with mental health symptoms is significant. This can further complicate your health picture but also opens more avenues for a VA secondary claim.
PTSD, Depression, Anxiety And Sleep Apnea
Sleep is usually one of the first things to fall apart when your brain stays stuck in survival mode. Many vets with PTSD or chronic anxiety later get diagnosed with obstructive sleep apnea.
The VA rate for sleep apnea is 0, 30, 50, or 100 percent under DC 6847 Sleep Apnea Syndromes. A CPAP prescription is often enough to fall in the 50 percent range. This can drastically change your overall VA disability rating.
To medically connect sleep apnea to a mental health condition, many veterans point their doctors to clinical research in sleep apnea studies. These show links between chronic stress, weight gain, disrupted sleep patterns, and apnea. Your doctor can then write a clear opinion stating that your service connected PTSD or anxiety at least as likely as not led to the sleep apnea or made it worse.
Migraines As A Secondary Condition To Mental Health
Migraines are another common piece of this puzzle. Veterans with long standing anxiety or depression often develop frequent, severe headaches over time. This becomes a viable VA secondary claim.
Research on migraines with aura, and data from places like the Mayo Clinic’s discussion of classic migraine, show higher rates of depression among migraine patients. That shared link gives your doctor scientific backing.
The VA rates migraines at 0, 10, 30, or 50 percent using DC 8100. To connect them secondarily, your doctor should document when the migraines began. They must explain how your mental health symptoms showed up and cite research showing the migraine and mood disorder connection.
Hypertension, GERD, IBS, And Other “Body” Problems From Stress
Chronic anxiety, hypervigilance, and sleep problems put pressure on your whole body. They can raise blood pressure, upset your gut, and throw your hormones off balance. These physical reactions are a legitimate medical condition resulting from mental strain.
A study highlighted on PubMed showed patients with anxiety and depression sometimes had better hypertension control only because they had more visits. That alone shows how often these conditions are linked in real patients.
The VA rates hypertension at 10, 20, 40, and 60 percent under DC 7101 Hypertensive Vascular Disease. To argue it as secondary, you can show blood pressure trends in your records that rise as your mental health worsens. Support this with studies in medical databases such as PubMed.
Gastro issues are similar. A 2023 study on GERD found about one in three people with reflux symptoms also live with anxiety or depression. GERD itself is rated under DC 7206, while IBS gets rated under DC 7319 with 10, 20, or 30 percent options.
Your GI doc or primary care provider can connect your service connected PTSD, depression, or anxiety to GERD or IBS. They do this by pointing to the timing of your symptoms and those mental health studies. The more your treatment notes show “stress flares” lining up with stomach problems, the stronger the link.
Bruxism And TMD From Anxiety
If you grind your teeth at night or clench your jaw all day, you might have bruxism or temporomandibular disorder. Many vets assume this is “just a bad habit,” but research shows a clear tie between these conditions and mental health.
Studies like the ones listed on this bruxism research page connect tooth grinding with emotional disorders and work stress. The VA rates TMD using DC 9905, with possible ratings between 10 and 50 percent depending on your jaw range of motion.
Your dentist or oral surgeon can help you build a secondary claim by explaining how long term clenching caused damage. Pair that with your mental health records and medical articles and you have a clear line. The argument is that PTSD or anxiety led to bruxism, which led to TMD.
2. Orthopedic Problems: The Chain Reaction Through Your Joints
If you have served with heavy rucks, bad boots, long marches, and hard landings, you know joint damage does not happen in a neat, single place. One bad knee leads to a bad hip, then low back pain, then neck pain, and so on. This is known as the kinetic chain.
Think about your body like a machine with linked parts. If one part fails, the strain lands somewhere else. Secondary joint conditions are often some of the most missed service-connected disabilities because vets blame age rather than service.
Knees, Hips, And Low Back
Say your left knee is rated at 20 percent from a service injury. Over time, you limp and shift weight to the right side. Now your right hip and low back are burning every day.
A strong secondary claim here comes from a doctor or physical therapist explaining the mechanics. They can write that your abnormal gait from the service-connected condition is at least as likely as not causing your back or hip arthritis. It may have caused it to develop sooner or worsened it beyond its natural course.
You can support that medical opinion with orthopedic research pulled from sources like PubMed. Those papers often talk about gait changes and the stress they put on the spine and joints. Getting disability compensation for these orthopedic chains is common if the evidence is clear.
Feet And Plantar Fasciitis
Many vets also deal with flat feet, plantar fasciitis, or chronic ankle strain that grows from existing knee, hip, or back problems. Once again, it is the chain reaction of the body.
A podiatrist can document how your foot structure or gait changed after the original injury. Their statement becomes the missing bridge between “I already have this rating” and “here is why this new problem counts as secondary.” This secondary service-connected disability claim is often won with a simple gait analysis letter.

3. Hearing Loss, Tinnitus, And Balance Problems
Hearing loss and tinnitus are two of the most common service connected disabilities. But what many veterans miss is that balance issues and even some types of headaches can show up as secondary to inner ear problems.
Your inner ear controls both hearing and balance. If you have tinnitus or hearing loss, it can sometimes lead to vertigo or frequent dizziness. This can affect your ability to work and lead to claims for VA disability compensation.
When you submit a claim for those symptoms, submitting clear evidence with your VA Form 21-526EZ makes a real difference. This is especially true if you are arguing secondary conditions to hearing loss such as tinnitus or balance disorders. The veterans affairs rating schedule recognizes these connections if the medical proof is there.

4. Erectile Dysfunction And Hormonal Issues
Few topics make vets more uncomfortable than sexual health. So ED tends to stay hidden and unclaimed, even when it clearly ties to service connected issues. Common causes include diabetes, PTSD, spinal damage, or medication side effects.
The VA usually rates erectile dysfunction at 0 percent, but that does not mean it has no value. ED can qualify you for special monthly compensation, which can bump your monthly pay. This is separate from your standard rating.
To build the link, you want your doctor or urologist to write a clear statement about what is causing the ED. They can point to spinal nerve damage, blood vessel disease, or the mental health medication you take. Studies listed in PubMed often back up these medication and disease connections, giving the opinion more strength.
5. Heart Disease As A Secondary Heavy Hitter
Heart disease hits veterans hard. Long term stress, high blood pressure, lack of sleep, tobacco use, and chronic pain all work against your heart over the years. These factors often stem from a primary service-connected disability.
The 2025 American Heart Association fact sheet shows heart disease staying near the top of leading causes of death in the United States. Veterans, with higher rates of hypertension, mental health conditions, and metabolic issues, often sit right in the danger zone.
You can connect heart disease as secondary to service connected hypertension, diabetes, or even long term sleep apnea. The goal is to show that those primary conditions existed for years and damaged your heart. The damage is then clearly tied in the record through lab results, stress tests, and specialist notes.

How To Medically Connect A Secondary Condition The Right Way
You might be thinking, “Okay, I see the links. But how do I prove it in a way VA cannot easily deny?” Here is a step by step approach many successful veterans use. This process works for a new claim or a supplemental claim.
Step 1: List Your Service Connected Conditions And Your Symptoms
Start by writing out your current service connected ratings and dates. Next, make a second list of symptoms and diagnoses you have now that are not service connected yet. Using a disability calculator can help you estimate how these potential new ratings might increase your total percentage.
Do you have trouble sleeping, constant heartburn, chronic headaches, jaw pain, ED, or dizziness? Put it all on paper, even if it feels unrelated. Identifying the primary service-connected condition that started it all is crucial.
Step 2: Research The Medical Links
This is where medical databases help. Go to PubMed and type in combinations such as “PTSD obstructive sleep apnea,” “anxiety hypertension,” or “knee osteoarthritis low back pain.”
You are not trying to become a doctor. You are gathering articles that show known links. These studies give your doctor and your future C&P examiner something objective to lean on for your service connection claim.
Step 3: Talk With Your Treating Doctors
Share what you found with your VA or private providers. Ask honest questions. Do they think your service connected PTSD likely led to your sleep apnea?
Do they see your old knee injury changing the way you walk and leading to back pain? Once a provider agrees with the link, ask for a clear written opinion. This is your nexus.
The opinion should use the right language: “it is at least as likely as not that the veteran’s X condition was caused by or aggravated by their service connected Y.” This phrase tracks with the rule under 38 CFR § 3.310 and supports your secondary service connection claim.
Step 4: File VA Form 21-526EZ For Your Secondary Claims
Veterans should submit secondary claims using VA Form 21-526EZ. You can file online through VA.gov or mail the paper version. This is the standard form for a VA disability claim.
On the form, make it clear each new condition is claimed as secondary to a specific service connected disability. Attach medical records, research printouts, and your doctor’s opinion letter. If you have a connection claim that was previously denied, you may need to file a supplemental claim with new evidence instead.
You can also open a new claim using the online application process explained here for the VA Form 21-526EZ Application for Disability Compensation and Related Compensation Benefits. Make sure you save copies of everything you submit. If you are aiming for a higher VA disability calculator result, accuracy here is vital.
Do “Most Common” Lists Help You Spot Missed Conditions
You have probably searched for lists of the most common secondary disabilities before. You will see the phrase most common all over the internet, used for all sorts of topics, like the most common sleep disorders, the most common sustainable materials, or even articles about the most common CCTV questions.
That phrase grabs attention, because our brains want quick patterns. In the veterans benefits space, you will also see “most common secondary claims” headlines shared widely in local news. For example, there is this repeat feature on Top 5 Secondary Service Connected Disabilities and how to claim them, echoed across outlets like the Winchester Sun and the Oxford Eagle.
Those pieces tend to mention conditions such as migraines, sleep apnea, radiculopathy, GERD, and secondary mental health ratings. They give a helpful checklist. But the real magic is not just seeing the list.
It is learning how to translate those broad patterns to your own medical record. You must build the bridge the VA has to respect.
Why This Matters For Your Future
This is about more than money. Missing secondary ratings can affect your access to care, family protections, and your choices as you age. It is a fundamental part of disability law for veterans.
Better ratings can help if your spouse or children later need benefits tied to your service. They can make long term health planning and things like estate decisions smoother, which groups like Bequest Management talk about when they cover planning for families in their resources. Access to va disability benefits can provide security for decades.
Secondary claims can also be the difference between scraping by and feeling like you finally have breathing room. And yes, it can give some peace of mind knowing your conditions are finally seen for what they really are. They are not just “getting older”; they are part of the sacrifice you made.

Conclusion
By now, you have seen how deep this rabbit hole runs. Most veterans leave a lot on the table because no one sat them down and walked them through the Most common secondary conditions veterans miss. How to medically connect them in a clear, human way.
Your job from here is not to memorize regulations. It is to look at your body and your mind honestly. Then match what you live with against what the medical research already shows in places like PubMed.
Look at what VA rules already allow through 38 CFR § 3.310. Most importantly, see what your doctors are willing to say on paper. If you do that work, get solid medical opinions, and submit organized claims with forms such as the VA Form 21-526EZ, you give yourself a real shot at success.
You can close the gap between how bad you feel and what VA has on file. The Most common secondary conditions veterans miss. How to medically connect them are no longer hidden once you shine light on them with facts, research, and your own story, told clearly and backed up the right way.

