VA Disability for Asthma. Which pulmonary tests strengthen a VA asthma claim? If you are asking that, you are probably already tired of fighting to breathe and fighting the VA at the same time. You might have done your time in uniform around dust, burn pits, fumes, or freezing air on a flight line. Now you are trying to convince a rater who has never been there that your shortness of breath is real and serious.
Here is the truth: the VA leans hard on numbers, not just your words. That is why VA Disability for Asthma. Which pulmonary tests strengthen a VA asthma claim? is such an important question. The right pulmonary function tests can turn a weak claim into a powerful one that actually matches how you live day to day.
Why Pulmonary Tests Matter So Much For VA Asthma Claims
The VA ratings system is built around test results. Feelings and symptoms matter, but they are usually not enough by themselves. A respiratory condition claim often requires objective medical evidence to be approved. For asthma, VA raters look straight to the rating schedule in the respiratory section of the regulations, listed in 38 CFR § 4.97. Asthma has its own diagnostic code there under 6602. This code dictates how every VA rating for this condition is assigned.
Your percentage is tied closely to how you do on a pulmonary function test. So the tests you complete and how they are documented can raise or sink your asthma rating. Without these tests, obtaining a proper VA disability percentage becomes very difficult. It is crucial to understand that respiratory conditions are rated on functionality. The VA wants to know how much your lungs are limited compared to a healthy person. This is why asthma VA claims rely so heavily on the specific numbers from your medical charts.
Quick Look At How The VA Rates Asthma
Asthma is rated based on breathing test numbers, medication use, and the frequency and severity of attacks. That is all spelled out under DC 6602. The disability benefit you receive depends entirely on which criteria you meet. If your asthma is mild, well controlled, and your lungs show normal pulmonary function, the VA might decide it lines up with only a 10 percent rating. This is the lowest compensable level for most disability benefits related to asthma. This level usually corresponds to intermittent inhalational therapy usage.
On the other end, if you have frequent attacks, require strong medications, or have episodes of respiratory failure, you can reach a 100% asthma VA rating. The VA disability rating system rewards higher percentages for those with severe functional loss. Understanding where you fall on this spectrum is the first step in managing your claim.

The Role Of PFT Numbers In Your Asthma Percentage
The VA looks at specific lung function values on your pulmonary tests. The main ones are Forced Expiratory Volume in one second and ratios between different breathing measures. These numbers determine your specific VA rate. The higher your forced expiratory volume (FEV-1) score is, the lower the VA tends to rate your asthma. So it helps you to understand what those numbers mean before you step into a Compensation and Pension exam. Lower scores often lead to higher VA ratings.
The schedule also allows higher ratings based on the kind and frequency of medications and whether a doctor has documented serious attacks or respiratory failure. That is why your treatment history and test results must work together in your file. This combination is what builds a successful va claim. If you suffer from a respiratory disorder, your clinical findings must paint a clear picture. The VA rates rely on specific cut-off points in your test results. Knowing these cut-offs can help you spot errors in your decision letter.
Core Pulmonary Function Tests That Strengthen A VA Asthma Claim
The VA relies on a few main pulmonary function tests to judge the severity of your asthma. These tests look cold and clinical, but they become powerful evidence if your symptoms are severe. Proper function testing provides the concrete data raters need. Most of them fall under the group of exams known as pulmonary function tests or PFTs. As the Johns Hopkins description of PFTs explains, these tests measure lung volume, capacity, airflow, and gas exchange. Pulmonary function testing is the gold standard for diagnosing a respiratory condition.
For VA asthma claims, a handful of specific values carry most of the weight. Your vital capacity and expiratory flow are scrutinized closely. These specific metrics are often the deciding factor in your final rating.
Forced Expiratory Volume In One Second FEV1
FEV1 is usually the star of the show for VA asthma claims. It tells the doctor how much air you can push out during the first second of a hard, fast exhale. This specific piece of function testing helps determine if you have an obstruction. The Forced Expiratory Volume in 1 explanation gives a simple breakdown of what this measure means in lung testing. For asthma, the lower that FEV1 value drops, the more it lines up with serious breathing limits. A significant drop supports a higher disability rating.
The VA asthma schedule under DC 6602 breaks rating levels down using FEV1 as a major factor. So if you do not have a reliable, properly performed FEV1 test, your claim is already at a disadvantage. Without this data, proving the severity of your lung disease is much harder.
FEV1 To FVC Ratio
The FEV1 score does not stand alone. Doctors and VA raters also look at the relationship between FEV1 and Forced Vital Capacity or FVC. This comparison is vital for assessing lung health. This is known as the FEV1 FVC ratio. The FEV-1/FVC ratio helps reveal obstruction in your airways. It is a critical component of pulmonary function tests.
Asthma is an obstructive disease, so a lower ratio can back up your diagnosis and support a higher rating level if the results fall within certain ranges tied to the rating schedule. This ratio confirms that your respiratory disorders are indeed causing blockage.
Peak Expiratory Flow PEF
Peak Expiratory Flow shows how fast you can push air out at the strongest point of your exhale. Doctors can measure this during formal PFTs or with a home meter. Consistent low readings can validate your subjective reports. The VA often relies on values like FEV1 first, but Peak Expiratory Flow readings are still useful. They give extra proof of flare ups and day to day breathing swings. This data is helpful for showing the frequency of asthma attacks.
If your home peak flow values stay low despite medication, you can bring that record to a Compensation & Pension exam to back up what your doctor sees in the clinic. Documenting these clinical findings over time creates a stronger case.
Other Important PFT Measures For Asthma
A full PFT panel shows more than FEV1 and PEF. It may include values like FVC and total lung capacity. These additional function tests provide a complete picture of your lung health. The important PFT measures page outlines the major lung values doctors look at during these tests. The VA focuses on a subset of those values for asthma, but other numbers still support the medical story. A comprehensive look at your vital capacity can rule out other issues.
Your job is not to memorize all of them. Your job is to make sure those test results end up in your VA file and match how you actually function in real life. Accurate medical records are your best tool.
How PFT Results Tie Directly To Asthma Rating Levels
The asthma rating schedule looks technical on paper, but the structure is fairly clear. Different PFT ranges and medication needs match different ratings under DC 6602. The nexus letter from your doctor can help explain these results to the VA.
That means each PFT you complete is an opportunity to lock in a higher rating or to lose ground if it is rushed, incomplete, or not repeated during a bad flare. If you suffer from a secondary condition, these tests help distinguish between overlapping symptoms. Understanding the requirements for each level helps you know what evidence to gather.
Here is a simple way to look at how pulmonary tests guide your rating level, based on how the schedule uses FEV1 and related values.
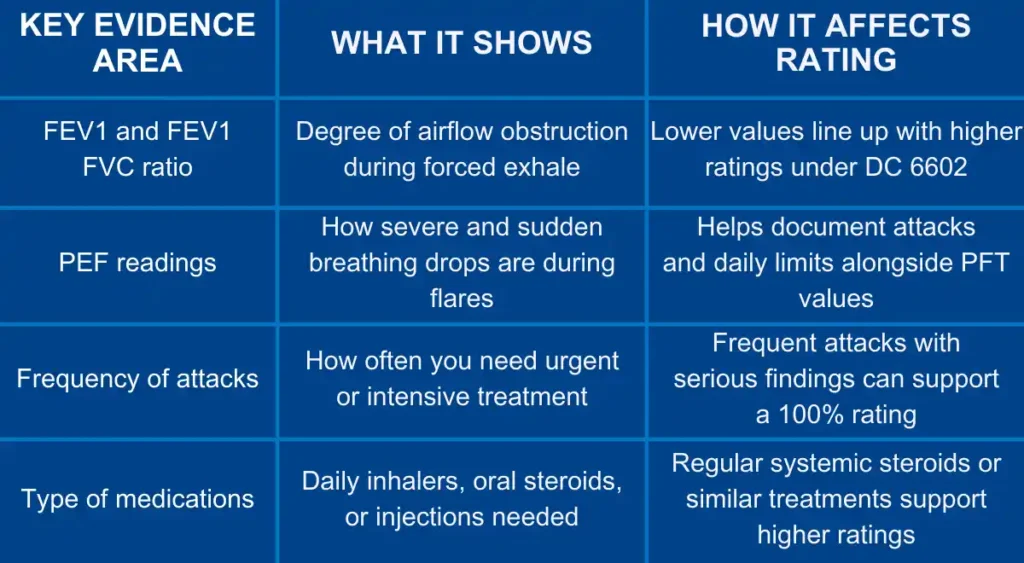
To get a 100% rating, you generally need to show FEV-1 of less than 40% predicted. Alternatively, having more than one attack per week with episodes of respiratory failure works too. Taking daily high dose corticosteroids or immuno-suppressive medications also qualifies for this top rating.
A 60% rating often involves an FEV-1 between 40 and 55% predicted. It can also be granted if you require monthly visits to a physician for required care of exacerbations. Intermittent courses (at least three per year) of systemic corticosteroids also fit here.
The 30% level usually requires an FEV-1 between 56 and 70% predicted. This rating is also common if you use daily inhalational or oral bronchodilator therapy. Even daily anti-inflammatory medication usage can justify this 30 percent evaluation.
For veterans who cannot work due to asthma, there is also another path. Even if your main asthma rating is less than 100%, you may qualify for TDIU benefits if the condition makes it impossible to hold gainful employment. This is a vital option for those with severe respiratory disorders.
Asthma, Exposure, And Why Veterans Face Higher Risk
If you feel like your breathing was fine before service, you are not imagining the change. Military environments can be rough on lungs. The stress on your respiratory system during service is real. Research has tied combat deployments and certain bases to higher rates of asthma and other respiratory problems. One of the biggest issues has been long term exposure to burn pits, which threw toxic particles and smoke into the air. Secondary conditions often arise from these toxic environments.
Recent studies have shown that service members exposed to burn pits, dust, and other airborne hazards carry a higher risk of developing asthma after deployment. Pit exposure creates long-lasting damage to lung tissue. This damage frequently leads to a diagnosable lung disease later in life. Burn pit exposure is a significant factor in modern veteran disability claims. The heavy smoke and chemicals inhaled during military service can trigger latent asthma or cause new onset symptoms. Documentation of where you served is critical for these cases.

The PACT Act And Asthma As A Presumptive Condition
Congress finally started to catch up to what veterans had been saying for years. Breathing in toxic air day after day comes with a price. This legislation opened the door for many VA disability benefits previously denied.
With the PACT Act passed in 2022, the VA began treating asthma as a presumptive condition for many post 9/11 veterans who served in certain locations and time periods. This means the rating criteria for service connection are easier to meet. You do not need to prove a specific incident caused the asthma if you meet the location requirements.
That means you may no longer have to prove the link between exposure and asthma from scratch if you meet the deployment criteria. You still need a clear diagnosis and solid tests, but the burden to show causation becomes lighter. This simplifies the va disability claim process significantly.
What Asthma Actually Does To Your Lungs
It can help to know what the doctors are seeing in those test numbers. Asthma is not just feeling winded during PT. It is a chronic lung disease that alters your physiology. As theasthma overview explains, asthma causes the airways to narrow, swell, and produce excess mucus. This makes it hard for air to flow in and out smoothly. These physical changes lead to the coughing and wheezing known as asthma symptoms.
Many veterans also deal with occupational asthma, triggered by exposures on the job. In service that might mean fuels, exhaust, chemicals, dust, or smoke during deployment or training. Secondary service connection can sometimes be established if another service-connected issue aggravates this condition. During an asthma attack, the airways constrict violently. This sudden change is what causes the drops in Peak Expiratory Flow. Documenting these attacks is key to proving the severity of your condition.
Other Respiratory Codes And Why They Matter
You might not have just asthma in your records. Many veterans carry a mix of respiratory issues, from sinus problems to chronic bronchitis. Having multiple respiratory disorders complicates the rating picture. The VA uses separate diagnostic codes under the respiratory section for these problems. The full list appears in 38 CFR § 4.97, where asthma is coded under 6602 but many other lung and upper airway issues sit beside it. Each condition has its own requirements for vital capacity or other metrics.
That list covers sinusitis under 6510–6514, chronic laryngitis under 6516, and allergic rhinitis under 6522, along with many more. Sometimes a veteran might have a secondary condition like sleep apnea linked to their respiratory state. Understanding the differences helps you file the right claim. The VBA report on compensation shows how common these respiratory codes are for veterans as a group. You are not the only one fighting these battles. Proper documentation of an in-service event is vital for any of these codes.

Asthma And Other VA Disability Claims Working Together
Your asthma claim does not sit on an island by itself. Many veterans also file for other conditions caused or worsened by service, or even made worse by asthma. This is where the concept of a secondary condition becomes relevant. For example, some veterans deal with gastro issues and acid reflux, which can irritate asthma. There are helpful breakdowns of VA disability ratings for hiatal hernia that show how those conditions are judged and rated. Acid reflux can actually trigger more frequent asthma symptoms.
Others fight joint pain that keeps them from staying active, like shoulder issues. A guide to shoulder related VA disability ratings can help you see how those claims line up next to your asthma claim. Reduced activity from joint pain can impact your cardiovascular and respiratory health. Women veterans often face under recognized conditions, including gynecological problems that may affect daily life and work. Resources explaining gynecological VA disability ratings help build the bigger picture of your full disability profile, not just your lungs. All these pieces, including secondary conditions, form your total disability percentage.
Step By Step: Building A Strong Asthma Claim With Pulmonary Tests
Once you understand which pulmonary tests matter most, the next step is to use that knowledge. You want your claim to tell a clear story, backed by strong evidence at every point. This process is about establishing service connection firmly.
Here is a simple plan that many veterans follow to give their asthma claim the best chance. Following these steps helps organize your medical evidence.
1. Confirm You Have A Current Asthma Diagnosis
VA ratings start with a clear diagnosis. A doctor must put asthma in your medical record. Without a current diagnosis, the VA cannot grant service connection. If your primary care notes just mention “wheezing” or “shortness of breath” but no confirmed diagnosis, you are missing a core piece. The asthma overview gives a basic sense of how doctors diagnose it, using symptoms and tests together. You need a doctor to state clearly that you have asthma.
Ask your provider directly whether your symptoms meet the medical standards for asthma and make sure the word itself appears in your chart if that is the case. This is the foundation of your service-connected disability claim.
2. Get Full Pulmonary Function Testing Done Correctly
Partial testing can hurt your claim. You want a complete PFT set performed and interpreted by someone trained in these exams. Establishing service requires comprehensive data.
The PFT session should include FEV1, FVC, the FEV-1/FVC ratio, and related values listed in PFT references such as those noted for important PFT measures. These values are the clinical findings the rater will look for first.
Try to schedule testing at a time when you have been breathing at your usual worst rather than right after a strong medication adjustment that makes your lungs look better on paper than in real life. Accurate medical records reflect your true condition, not just your best days.

3. Track Asthma Attacks, Triggers, And Treatment
Pulmonary tests are not the only thing that matters. The VA also pays attention to the frequency of your flare ups and the medications you rely on. Tracking your asthma attacks creates a timeline of severity.
Keep a simple journal that lists what triggers your asthma, how often you need rescue inhalers, and any urgent or emergency visits. The more specific the entries, the more useful they become for your doctor and your claim. This is especially true if you are on oral bronchodilator therapy.
If your doctor puts you on oral steroids, injections, or other strong treatments, ask that this is documented clearly as ongoing management for asthma rather than just a single flare up. Long-term use of anti-inflammatory medication or high dose corticosteroids is a major factor in higher ratings.
4. Connect Asthma To Your Service Or PACT Act Criteria
You have to show either direct connection to service or qualify through the presumptive path. Both roads still rest on your medical evidence. To prove service connection, you need to link your current condition to your time in uniform.
If you are claiming a direct service connection, your service records matter. You will usually need your DD 214 to show where and when you served and what your role was. This helps prove you had an in-service event or exposure.
For post 9 11 veterans in certain locations, the PACT Act can take some of that burden off. Asthma can be treated as presumed service connected for those who meet those criteria, which is a major relief for many burn pit exposed veterans. This helps prove service without needing a specific incident report.
5. File Your Claim With Supporting Forms And Statements
To get the VA to look at your asthma case, you need to start the claim with the correct paperwork. The main form used to begin a disability claim is VA Form 21-526EZ. This initiates the review of your VA disability benefits.
Once the claim is open, it can help to submit lay statements from yourself and from people who have seen you struggle. Use VA Form 21-10210 for those supporting statements from family, friends, or coworkers. These statements add personal context to your medical evidence.
Attach your best pulmonary test reports, clinic notes showing asthma diagnosis, and any records showing treatment after exposure during service or deployment. A nexus letter from a private doctor can also be very powerful here to connect your condition to service.
How Asthma Fits Within Your Larger Respiratory Picture
A lot of veterans discover they have more than one respiratory issue once they dig through their medical records. You may have sinusitis, chronic bronchitis, or sleep apnea along with asthma. These respiratory conditions often occur together.
The respiratory rating rules in 38 CFR § 4.97 cover a long list of codes for different conditions. Those codes include chronic bronchitis under 6600, bronchiectasis under 6601, and COPD under 6604. Knowing the correct code is essential for an accurate VA rate.
You cannot usually stack multiple ratings for conditions that affect the same lung function area. But it is still important that each problem is correctly named and coded so the VA can decide which route gives you the strongest benefit. Sometimes a rating for respiratory failure or another lung disease provides a better outcome than asthma alone.
How Pulmonary Testing Impacts Work And TDIU
Pulmonary test results do not just drive your base asthma percentage. They also become key proof in a claim for Individual Unemployability. This disability benefit is for those whose service-connected conditions prevent work.
If your lungs prevent you from performing any job that fits your background and skills, the VA may grant TDIU benefits. That benefit pays you at the 100 percent rate even if your combined ratings add up to less on paper. Severe respiratory conditions are a common basis for TDIU.
PFT numbers showing severe obstruction, along with doctor opinions and work history, can make the difference between a denied TDIU claim and a grant. If you require oxygen therapy or have extremely low vital capacity, working may be impossible.
Conclusion
If you started this search by typing VA Disability for Asthma. Which pulmonary tests strengthen a VA asthma claim?, you probably knew that breathing tests mattered, but maybe not how much. The process of securing VA disability benefits for asthma hinges on these objective measures.
The bottom line is simple. Strong, clear pulmonary function tests, combined with an accurate asthma diagnosis, exposure history, and detailed treatment records, can turn your claim into a well supported package that speaks the VA’s language. Your daily inhalational medication logs and PFT scores are your best allies.
You gave your lungs during service. Now the PFT numbers, diagnostic code 6602, and your medical records together can help you claim the rating you have earned and the stability you deserve from the VA disability system. Whether through direct service connection or as a presumptive condition, you have a path forward.