If you are searching for how to prove a VA claim for vertigo after TBI. evidence needed for VA balance disorder claim, you are probably tired. You might be tired of feeling the room spin without warning. You are likely tired of gripping walls just to walk down a hallway safely. And you are certainly tired of receiving VA decisions that do not match how bad your life feels day to day.
You are not alone in this struggle. Many veterans deal with vertigo and balance problems after a head injury and have no idea how to prove a VA claim for vertigo after TBI. evidence needed for VA balance disorder claim in a way that makes sense to VA. The good news is that there is a clear way to build the medical record.
Once you understand what the Department of Veterans Affairs wants to see, things start to feel a lot less random. It requires specific pieces of medical evidence and a clear link to your service. We will break down exactly how to organize your claim.
Why Vertigo After TBI Is So Hard To Explain To VA
Vertigo and balance issues after a head injury are real, but they can be invisible on a simple exam. You can feel like the floor moves under your feet while your doctor sees normal lab work. You might have a steady walk on that one good day you came in for an appointment.
That gap between how you feel and what is on paper is where many VA claims fall apart. Your job is to close that gap with clear, consistent evidence and the right wording. VA has rules that recognize traumatic brain injury and related problems like vertigo.
However, the rules need to be used correctly to get the right disability rating. VA rating rules for traumatic brain injury live in 38 CFR 4.124a, DC 8045. That regulation explains that an external force to the head can lead to both direct brain injury and separate physical or mental problems.
This is exactly what many veterans with vertigo live with every day. The damage from a TBI can be complex. It often involves more than just cognitive impairment or memory loss.
How Vertigo Fits Into VA’s Rules For TBI
After a TBI, VA rates many symptoms under a table called Evaluation of Cognitive Impairment and Other Residuals of TBI Not Otherwise Classified. Vertigo often lands in what VA calls the subjective symptoms area under that same TBI rule at DC 8045. This area is designed to capture physical sensations that are hard to measure.
VA guidance explains that if a veteran has vertigo, no matter if it is called peripheral vestibular disorder or positional vertigo, it can be rated as a symptom under that TBI table. This simplifies things for some veterans. However, it can also lead to a lower rating if the rater groups everything together.
If doctors diagnose a separate condition that affects your ear or balance system, that condition can sometimes be rated under another code. This applies as long as VA avoids rating the exact same symptom twice. You have to be careful about how you present this information.
This is where rules on pyramiding under 38 CFR 4.14 come in. VA is told not to rate the same symptom two different ways. However, VA can rate separate conditions when they cause different problems in your life.
Service Connection Basics For Vertigo After TBI
Before you worry about rating percentages, you need service connection. Without that, there is no monthly payment no matter how bad your vertigo feels. Establishing a service-connected condition is the first hurdle you must clear.
For direct service connection under 38 CFR 3.303, VA looks for three things. First, you need a current diagnosis or clear ongoing symptoms of a vertigo condition. Second, you must show a documented in-service event or injury such as blast exposure, fall, vehicle crash, or impact.
Third, you need a medical opinion that links the current vertigo to that in-service TBI. This link is often called a nexus. The same rule explains that if there is a formal TBI diagnosis tied to service, you can still get service connection even if a later exam claims the TBI has resolved.
The focus is the link between what happened in service and the current residuals. Vertigo, headaches, and balance problems count as residuals when backed by a doctor and consistent history. This is true even for mild TBI cases where the initial injury seemed minor.
How To Prove A VA Claim For Vertigo After TBI. Evidence Needed For VA Balance Disorder Claim
To build a strong case, think like a rater reading your file on a busy afternoon. They see stacks of claims and move fast. Your evidence should tell a clear story on its own. Even a stranger should be able to follow how your vertigo began. They need to see how often it hits you. They must understand how it affects your work and daily life.
Your core evidence falls into a few groups. You need strong medical records and correct VA claim forms. You might need private expert opinions and lay evidence. Sometimes you will rely on rating rules that match your exact symptoms. Each group plays a role in the disability determination process. If one piece is missing, the whole claim might fail.

1. Start With The Right VA Claim Form
The first brick in the wall is your initial claim form. VA uses VA Form 21-526 for most new disability claims. On that form, you will want to be very clear that you are claiming vertigo and balance problems. State clearly that these are due to a service-connected TBI. You can also claim them as part of that TBI claim itself. If you already have TBI service connected but not vertigo, you can file for an increase.
You can also file for vertigo as a secondary condition. But do not assume VA will connect the dots for you. Write the words head injury, concussion, blast, fall, or whatever fits your history. Spell out that you have spinning, near falls, and balance trouble since that event. Be specific about your military service and when the injury happened. The more details you provide on the form, the better.
2. Medical Records And Objective Evidence
Medical documentation is the backbone of any claim that involves vertigo or a balance disorder. VA and outside research have shown that problems in the inner ear can cause serious balance problems. This includes dizziness, falls, and the classic spinning room feeling. Your records might include structural imaging like MRI or CT scans. You should include hearing tests and vestibular function tests. Notes from neurology or ENT visits are vital medical evidence.
Even if those tests are sometimes normal, repeated complaints over time in your chart help VA see that this is a long-term problem. It shows it is not just a short-lived episode. VA and private doctors also track symptoms such as unsteady gait. They look for positive balance tests and reports of nausea with head movement. Write down these symptoms after each visit. Make sure they appear in your treatment notes so the pattern is clear on paper.
If you suffer from benign paroxysmal positional vertigo, make sure that specific name is in the records. Benign paroxysmal positional vertigo is a very specific type of vertigo often caused by head trauma. Having this diagnosis can strengthen the link to a head injury.
3. Private Experts And Independent Exams
Sometimes VA exams are quick, and your story gets lost between checkboxes. In more complex cases, a strong independent medical opinion can shift the whole claim. This is especially true when dealing with the complexities of TBI residuals.
For many veterans, working with a reliable medical group that understands the VA claim process changes the game. Groups like Attain Med Group explain how a well-built claim often needs a specialist who can clearly tie your vertigo to your TBI. A specialist can list all current symptoms and explain how they limit work and daily life.
If mental health problems like depression or anxiety grew worse after the TBI and vertigo, an independent psychological opinion may also help. You might be dealing with a mental disorder that developed because of your physical limitations. Detailed exams like the ones described in this guide to va claim exams can support both emotional and cognitive residuals. These reports explain how everything fits together instead of treating each issue like it lives in its own box. They can address executive function issues alongside physical dizziness. A nexus letter from a private expert can be the key to winning.
4. Understanding What Counts As Strong Evidence
Good evidence for a vertigo or balance disorder claim is clear, specific, and consistent over time. You are not trying to sound dramatic. You are trying to be precise about your experiencing vertigo. Think about what accident lawyers look for after a truck crash. Guides that explain the evidence needed to win those cases talk about scene photos and expert reports. They rely on witness accounts and medical files.
The same idea applies here. You are building a case file that shows cause and effect. That is why learning about the kind of evidence needed to support an injury claim can help shift how you see your own VA file. Each note, exam, and statement adds a piece of proof that your vertigo is tied to that TBI. This accumulation of proof makes it harder for the VA to deny the claim. It helps verify your service records match your current condition.
5. Lay Statements From You And People Around You
Do not underestimate plain language statements from you, your spouse, family, or coworkers. VA calls this lay evidence. It matters more than many veterans think. Your statement should cover how often you feel dizzy. Explain what triggers it and how long the episodes last. Describe what has changed over the years. You might explain that you avoid ladders now. Perhaps you had to stop driving at night because of sudden spinning when turning your head. These details illustrate social interaction limitations and work restrictions.
Family or friend statements help paint the before and after picture. They can talk about you needing help in the shower or grabbing walls. They might notice you sitting down to avoid passing out. They can report you having to leave events because of sudden dizziness. The more real details provided, the better the rater can see how deep this runs. This personalizes the disability compensation claim.
How VA Rates Vertigo And Balance Disorders Linked To TBI
Once VA accepts that your vertigo is connected to service, the next step is figuring out the right rating. That rating drives your monthly payment. It also opens doors to more care and benefits. VA has several rating paths that can touch vertigo and balance problems. For TBI, the main rule is DC 8045. For some ear-based conditions that come with vertigo, VA may use the Meniere’s code.
This code is DC 6205 – Meniere’s syndrome (endolymphatic hydrops). Understanding how VA rates vertigo is essential for maximizing your benefits. Different codes result in different compensation levels.
TBI Rating Table And Vertigo
Under the TBI rating system, vertigo often shows up in the subjective symptoms area of the table. VA looks at how often the symptoms occur. They check how much they interfere with work or everyday tasks. They also determine if they limit basic functions like standing, walking, or driving. The TBI rule also makes clear that if you have other conditions with distinct diagnoses, those may be rated apart from the core TBI. The manual guidance in the VA system at V.iii.12.B.2.c explains this.
A veteran can get separate evaluations for comorbid mental, neurologic, or other physical disorders. This applies as long as the symptoms do not fully overlap. This is important for secondary conditions. This means if your vertigo has its own diagnosis, it might be rated separately. If your depression or headaches are diagnosed as separate conditions, each one might support its own rating. This works if the signs are different and described clearly.
Meniere’s Syndrome And High Vertigo Ratings
Some veterans develop a pattern of vertigo, hearing loss, and strange walking patterns after TBI. This pattern matches Meniere’s type symptoms. VA rates that pattern under DC 6205 – Meniere’s syndrome (endolymphatic hydrops).
Even if you do not have Meniere’s disease specifically, VA rates vertigo based on this code if the symptoms are similar. This includes peripheral vestibular disorders that cause dizziness.
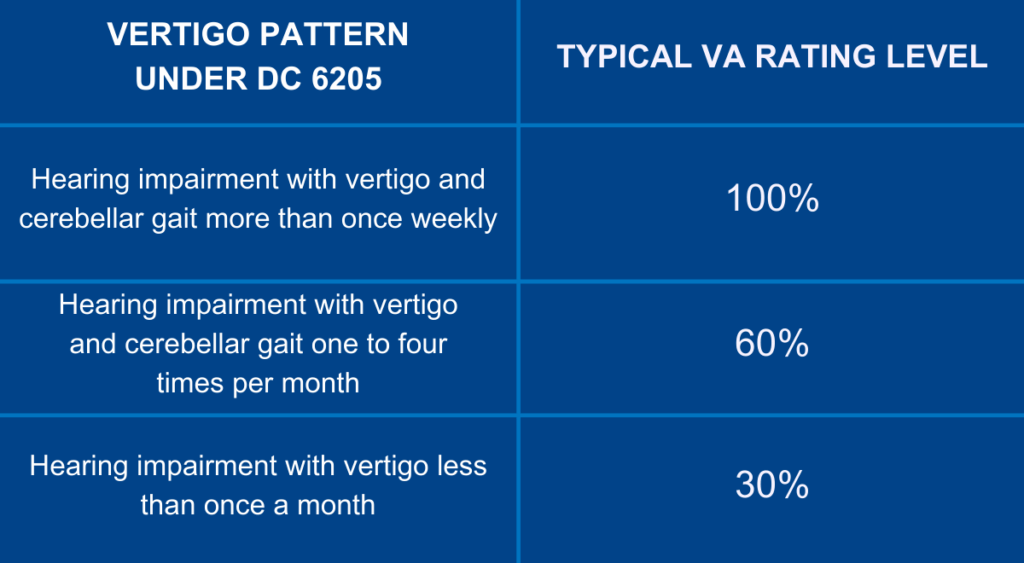
You will notice this rating path leans heavily on how often you have attacks. It also considers whether you have hearing changes and gait problems. Detailed tracking of your episodes is crucial. Hearing tests and notes about your walking pattern are also vital. This is especially true if your symptoms look anything like this picture. Documentation of paroxysmal positional attacks is helpful here.
Avoiding Pyramiding And Using The Right Codes
VA is not allowed to count the same symptom twice under different rules. This is called pyramiding. The bar against it lives at 38 CFR 4.14. But this does not mean you are stuck with one flat rating for everything after a TBI. VA guidance tells raters they can assign separate ratings for different conditions. This works if they come from a TBI and have clear, distinct diagnoses.
So you may see one rating under DC 8045 for cognitive or subjective symptoms. This could cover mild memory trouble. You might see another rating for migraines under DC 8100. Yet another rating could be for tinnitus under DC 6260. If your examiner cannot tell which symptoms belong to TBI and which belong to a separate mental health diagnosis, the rules change. DC 9434 tells VA to choose a single rating that reflects overall impact.
They must use the higher scale. But where possible, clear exam reports give VA more room. They can assign separate disability ratings and combine them under 38 CFR 4.25.
How Balance Disorders Are Defined And Proved
Many veterans know the feeling of almost tipping over when turning fast. You might feel it standing up too quickly or walking in the dark. But describing those moments to a rater who has never felt it is tough. Health sites give a helpful picture of what a balance disorder looks like in simple language. They list signs like unsteadiness and spinning feelings. They mention blurry vision when moving the head and frequent falls.
This same picture is what your evidence needs to show through notes. You need test results and real stories. Your job is not to copy those descriptions. You must show how they match your life. For example, maybe you get a wave of dizziness when you roll out of bed. Or perhaps you tilt your head to look up at a shelf and feel sick. Maybe your balance goes out on uneven ground. This makes even yard work risky. These examples illustrate the severity of your vertigo condition.

Linking Your Balance Problems Back To TBI
Some vertigo and balance problems come directly from ear injuries or illnesses that started later. Others are a delayed effect of TBI. The rules in 38 CFR 3.303 allow service connection either on a direct basis or as a secondary issue. If your vertigo and balance issues showed up shortly after a documented blast, fall, or impact, the link is usually more clear. When symptoms develop later, it helps to have a specialist. You need someone who can explain how TBI can disrupt the inner ear.
They can explain how it affects brain systems that handle balance. A cranial nerve injury might be the root cause. Specifically, damage to the eighth cranial nerve can lead to these issues. Again, this is where a strong independent medical opinion helps. A specialist report from a group that understands VA rules can close the gap. It connects your story and the paper record.
Understanding Benign Paroxysmal Positional Vertigo (BPPV)
One specific condition that frequently appears after head trauma is benign paroxysmal positional vertigo. It is often referred to as BPPV. This occurs when small crystals in the inner ear are dislodged by a blow to the head. When you include benign paroxysmal positional vertigo in your claim, you are being very specific. The word “benign” means it is not life-threatening, but it is certainly life-altering. “Paroxysmal” means it comes in sudden, brief spells.
“Positional” means it is triggered by certain head positions. If you include benign paroxysmal in your diagnosis, it helps explain why your dizziness is triggered by movement. Doctors can test for paroxysmal positional vertigo using specific maneuvers. Having a diagnosis of benign paroxysmal positional can strongly support a claim based on head trauma. It creates a clear mechanical link between the impact and the symptom.
Vertigo, Work Problems, And TDIU
For some veterans, vertigo and balance problems go far beyond inconvenience. They stop you from doing basic job tasks. This is especially true for tasks that involve ladders, heights, driving, or fast head movements. If your combined ratings are high, but you still cannot hold gainful work, you have options. TBI residuals and vertigo can lead to Total Disability based on Individual Unemployability, or TDIU. VA can pay you at the 100 percent rate.
This happens when your ratings meet certain levels and you cannot keep steady employment. Schedular TDIU calls for either one condition rated at least 60%. Alternatively, you can have several conditions with one at least 40 percent and a total of at least 70% combined. The rule at 38 CFR § 4.16a spells those numbers out. Vertigo linked to TBI may be one of the main pieces in that combined picture. This is especially true when it limits work around equipment or vehicles.
Impairment of executive functions combined with vertigo makes office work hard too. You might not be able to look at screens or focus. This strengthens the argument for unemployability.
Special Temporary Ratings For Serious TBI Cases
Some TBI cases involve long hospital stays or long recovery times where work is completely off the table. VA rules recognize this kind of unstable situation with temporary high ratings. These can provide a financial bridge during recovery. VA can grant prestabilization ratings at 50% or 100% after discharge. This applies when a veteran’s condition is very severe and not yet stable, under 38 CFR 4.28. For extended hospital care or major surgery, different rules apply.
VA can use temporary total ratings based on 38 CFR 4.29 and 38 CFR 4.30. While these rules may not apply to every vertigo case, they matter if you had a very rough course. If you had long rehab or surgeries related to head or ear damage, check these rules. It is easy for VA to miss these unless they are pointed out. They must be backed by hospital records. Make sure your representative looks for these opportunities.
Note also that if your TBI rating is based on an older set of rules from before October 23, 2008, you have rights. You can ask VA to review the rating under the current standard described in DC 8045. The note section explains that this request can be made at any time.

Practical Steps To Strengthen Your Vertigo And Balance Disorder Claim
It is easy to get lost in codes and legal sections. Let’s bring it back to clear steps you can start on this week. Think of these as real actions that bring your case closer to what VA needs.
Track Your Symptoms Daily
Start a simple paper or phone journal for at least 30 days. Every time you feel dizzy, write the time. Note what you were doing. Record how long it lasted. Write down what you had to stop or avoid. Patterns in this journal will support your own statement. They help your doctor understand triggers. They show the rater that your vertigo is frequent and disruptive. This can matter for ratings under TBI. It is also vital for any consideration under codes that look at episode frequency. This includes the Meniere’s rating code. Data makes your claim undeniable.
Bring Printed Rules Or Notes To Your Exam
Doctors are busy and may not think about VA rules while they talk to you. Bringing a short note can help. Explain you have a TBI, vertigo, and concerns about balance. State clearly that these affect work and daily life. You can guide the visit this way. You do not need to argue about diagnostic codes.
But you can mention that TBI residuals such as vertigo are listed in DC 8045. Mention that you hope the exam report notes frequency and impact in detail. A Disability Benefits Questionnaire (DBQ) usually asks these questions, but extra notes help. Small nudges like this help doctors write reports. These reports answer the questions VA is trained to ask. It ensures nothing is missed.
Consider Specialist And Independent Opinions
If VA has denied your claim once or more, look outside the system. It may be time to think about support outside the standard process. Some medical groups build their entire practice around veteran exams. They specialize in records reviews and expert letters. A group such as Attain Med Group focuses on helping build a strong claim. They do this through careful evaluation.
They can offer in-depth testing and a narrative opinion. This connects the dots in ways short VA exams do not. For mental health layers like depression tied to chronic dizziness, this is crucial. Services built around va claim psychological exams can fill key gaps. These reports are not magic, but they give VA more to work with. They often spell out clear cause and effect. They show how each diagnosis fits the rating rules. This makes it harder for VA to overlook the full picture. It creates a robust file.
Conclusion
Living with vertigo and balance problems after a head injury is hard enough. Having to learn how to prove a VA claim for vertigo after TBI. evidence needed for VA balance disorder claim on top of that can feel unfair. But knowing the rules and building the right kind of record does shift things in your favor. VA law already recognizes that a traumatic brain injury can cause separate physical and emotional issues. This includes dizziness and balance problems, under DC 8045 and 38 CFR 3.303. Your mission is to match your evidence to those rules.
Start with clear claims on VA Form 21-526. Use strong medical and lay statements. Where needed, obtain independent opinions to explain the nexus. If you take nothing else away, remember this one thing. Describe your vertigo in specific detail and connect it to your in-service TBI. Back it with records that show ongoing impact on work and daily life.
That is how you move from frustration to a successful outcome. You can build a claim that finally shows VA exactly how much this balance disorder has cost you. With the right evidence, you can get the benefits you earned.