Numbness and neuropathy are commonly dismissed by the VA. Learn how to document symptoms, triggers, and medical findings to prove your claim.
Many veterans experience numbness, tingling, or burning sensations in their arms or legs—but these symptoms are often underrated in VA disability claims. Whether due to peripheral neuropathy, radiculopathy, toxin exposure, or a service‐connected condition like diabetes, these nerve-based issues can be just as disabling as pain or mobility problems.
At Attain Med Group, we know how vital detailed, well‑documented medical evidence is to obtaining service connection (or a higher VA rating) for neuropathy. In this guide, we walk you through what the VA considers “strong evidence”, how to prepare your claim, and how to work with clinicians to build a winning case.

1. Understanding Neuropathy & Numbness in VA Claims
What Is Peripheral Neuropathy?
- Peripheral neuropathy refers to damage or dysfunction of peripheral nerves, which can lead to symptoms like numbness, tingling (paresthesia), burning, weakness, or loss of sensation.
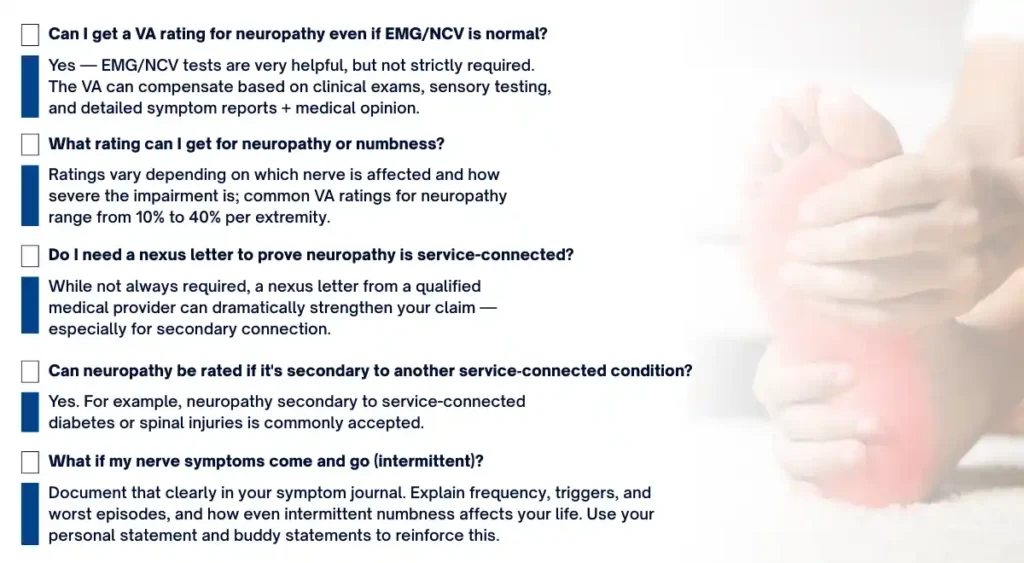
- The VA does not have a single diagnostic code labeled “peripheral neuropathy.” Instead, neuropathy is rated analogously, often under diagnostic codes for nerve paralysis, neuritis, or neuralgia depending on which nerves are affected.
- For example, sciatic nerve involvement may be rated under Diagnostic Code (DC) 8520 (paralysis of the sciatic nerve).
Why the VA Sometimes Dismisses Numbness
- Sensory symptoms like “numbness” or “pins-and-needles” may not show up clearly in standard physical exams, especially if motor function (muscle strength) is preserved.
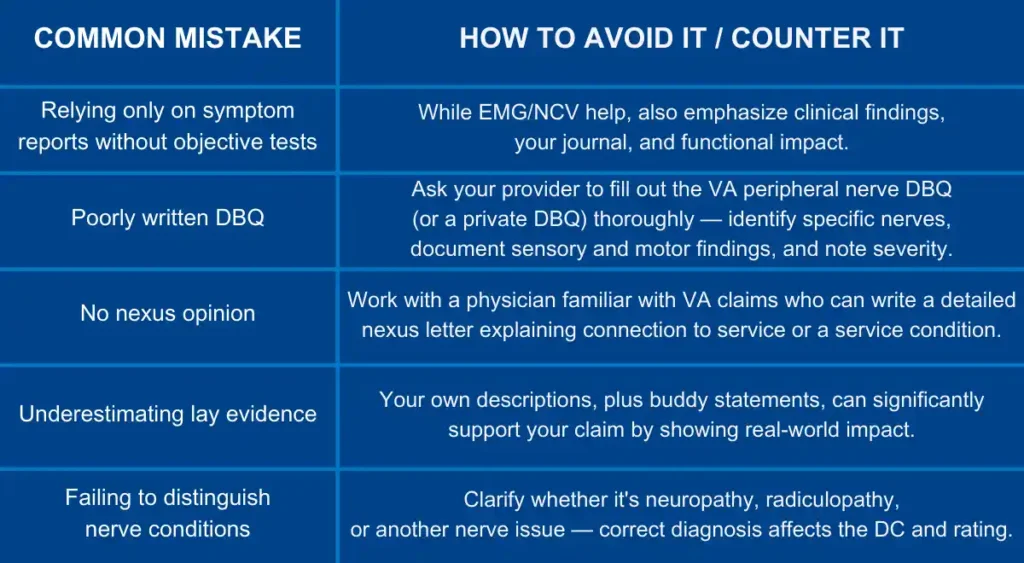
- VA examiners may under-evaluate or misclassify sensory neuropathy, particularly without objective testing like nerve conduction studies. Veteran advocacy groups argue that newer rating criteria should better account for sensory loss such as paresthesia or dysesthesia (abnormal sensation).
- Because of this, medical documentation, symptom reports, and expert opinions become especially important in establishing and proving your disability.
2. How the VA Rates Neuropathy & Numbness
To maximize your rating, you need to know how the VA evaluates and assigns ratings for nerve-related disabilities.
Rating Structure & Diagnostic Codes
- The VA uses Diagnostic Codes (DCs) to rate nerve conditions, depending on which nerve or group of nerves is involved.
- Severity is often tied to whether there is “complete” or “incomplete” paralysis (i.e., loss) of sensory and/or motor function.
- Under proposed changes, VA may define:
- Incomplete sensory neuropathy: sensation is impaired (but not absent) — includes numbness, dysesthesia, paresthesia.
- Complete sensory neuropathy: loss of sensation.
- Incomplete sensory neuropathy: sensation is impaired (but not absent) — includes numbness, dysesthesia, paresthesia.
Sample VA Ratings for Peripheral Nerves
According to VA rating guides:
Mild sensory / incomplete impairment → lower ratings (e.g., 10%)
Moderate to severe impairment → higher ratings, depending on which nerve(s) are affected and whether motor function is involved
Bilateral factor: if both limbs are affected (e.g., both legs) the VA may apply a bilateral rating factor, increasing total disability.
Radiculopathy vs. Neuropathy
- Sometimes, what feels like “neuropathy” is actually radiculopathy — nerve root compression (e.g., from a herniated disc). VA has specific rating criteria based on which nerve roots (C‑, T‑, L‑) are affected.
- Properly distinguishing between these conditions through diagnosis is critical, since it affects which DCs VA uses and how major or minor your rating can be.
3. What Counts as Strong Evidence for a Neuropathy Claim
To make your claim compelling, you need a robust evidence package. Here are the key types of evidence the VA looks for:
A. Clinical / Diagnostic Evidence
- Medical Diagnosis
- A clinician’s diagnosis of neuropathy, neuritis, or related nerve condition should appear in your medical records. Use VA or private records — whatever reflects your reality.
- A clinician’s diagnosis of neuropathy, neuritis, or related nerve condition should appear in your medical records. Use VA or private records — whatever reflects your reality.
- Objective Testing
- Electromyography (EMG) and Nerve Conduction Velocity (NCV) studies are extremely valuable. These tests measure how well your nerves conduct electrical signals, showing abnormalities.
- If available, quantitative sensory testing (QST) or autonomic testing can further support nerve damage documentation.
- Even if EMG/NCV is not performed, the VA recognizes other clinical findings such as: sensory testing (light touch), deep tendon reflex changes, muscle atrophy, gait abnormalities.
- Electromyography (EMG) and Nerve Conduction Velocity (NCV) studies are extremely valuable. These tests measure how well your nerves conduct electrical signals, showing abnormalities.
- Disability Benefits Questionnaire (DBQ)
- Use the VA “Peripheral Nerve Conditions” DBQ. This DBQ includes sections for symptom history, diagnosis, and functional impairment.
- Make sure your provider completes it fully — noting which nerves are affected, how symptoms present (numbness, pain, paresthesia), and whether they are constant or intermittent.
- Use the VA “Peripheral Nerve Conditions” DBQ. This DBQ includes sections for symptom history, diagnosis, and functional impairment.
B. Nexus / Medical Opinion
- A nexus letter (expert medical opinion) is often the linchpin of your claim: a physician should explain how your neuropathy is related to service (direct), or to a service-connected condition (secondary), or to in-service exposure/injury.
- The nexus should clearly articulate “at least as likely as not” (50% or greater probability) that your neuropathy is connected to your service or a service‑connected disability.
- It should reference your medical history, symptom progression, clinical findings, and test results.
C. Symptom & Functional Evidence
- Lay Statements / Personal Journal
- Keep a daily symptom journal: record how often you feel numbness, tingling, burning; note when it happens, which limbs are affected, intensity, and what makes it worse or better.
- Describe how numbness impacts your daily life: balance, walking, fine motor tasks, sleep, strength.
- Keep a daily symptom journal: record how often you feel numbness, tingling, burning; note when it happens, which limbs are affected, intensity, and what makes it worse or better.
- Buddy Statements
- Ask family, friends, or fellow service members to write statements about how they’ve observed these symptoms in you (e.g., “He hesitates when walking downstairs because his legs feel numb,” or, “She can’t grip small objects because of the tingling in her fingers”).
- Ask family, friends, or fellow service members to write statements about how they’ve observed these symptoms in you (e.g., “He hesitates when walking downstairs because his legs feel numb,” or, “She can’t grip small objects because of the tingling in her fingers”).
- Treatment Records
- Document all treatments you’ve tried: medications (e.g., gabapentin, pregabalin), physical therapy, assistive devices, or even home remedies.
- Show any follow-up notes, prescriptions, side effects, and how effective (or ineffective) treatment has been.
- Document all treatments you’ve tried: medications (e.g., gabapentin, pregabalin), physical therapy, assistive devices, or even home remedies.
4. How to Prepare for Your C&P Exam & Strengthen Your Claim
To maximize your chances at the C&P (Compensation & Pension) exam, preparation is critical.
- Bring your journal: Take your symptom log to the exam — point out patterns (times of day, triggers, duration).
- Bring buddy statements or personal/family observations: These help show functional impairment beyond what you tell the examiner.
- Ask the examiner to test sensation: Use light touch, pinprick, or other sensory exams. Make sure they record where you feel numbness and whether it’s partial or complete.
- Don’t rely solely on EMG: Even if EMG/NCV was normal (or not done), your symptoms + exam findings + nexus opinion can still support compensation. As veterans have reported:
“An advanced rater can discern that there is no rule requiring a positive EMG finding to award a claim … for neuropathy.” - Discuss functional impact: Explain how your nerve symptoms affect your daily tasks (walking, dexterity, balance, carrying things).

7. Why Working With Attain Med Group Makes the Difference
Navigating a neuropathy or numbness VA claim can feel overwhelming — but you don’t have to go it alone. Here’s how Attain Med Group supports you:
- Veteran‑Owned, Veteran‑Focused: We deeply understand the impact of these “invisible” nerve conditions and how VA rates them.
- Expert Medical Providers: We work with neurologists and other clinicians experienced in writing VA‑friendly nexus letters and completing DBQs.
- Comprehensive Document Review: We’ll review your service records, treatment notes, EMG/NCV results, and your symptom journal to build a strong medical narrative.
- Claims Strategy: We help you prepare for your C&P, gather lay statements, and organize the evidence in a way VA raters understand.
- Appeal & Supplemental Support: If you were denied or rated too low, we strategize how to strengthen your case with additional evidence or better medical opinion.
Conclusion & Call to Action
Numbness and neuropathy may feel “just uncomfortable,” but in the VA disability system, they can—and should—be taken seriously. With the right medical evidence, a well-written nexus letter, and a clear documentation of your symptoms and their impact, you can build a strong claim for service connection and increase your VA rating.
At Attain Med Group, we’re committed to helping veterans like you translate nerve symptoms into compelling, evidence-backed VA claims. Contact us today to schedule a free consultation. Let us help you build your case—with expert support through every step.
→ Book Your Consultation
→ Download Our Neuropathy Claim Checklist