When a veteran’s VA disability claim is denied—or receives a lower-than-deserved rating—the path forward often depends on submitting new and relevant evidence. Under the Appeals Modernization Act (AMA), this standard replaced the old “new and material evidence” requirement, making it clearer (and in many cases easier) for veterans to strengthen or reopen their claims.
But knowing exactly what the VA considers “new” and “relevant” is where many veterans get stuck.
This guide breaks down the evidence rules in plain language—so you know what counts, what doesn’t, and how expert-prepared medical evidence from providers like Attain Med Group can dramatically transform a denied or stalled claim.

What Does the VA Consider “New and Relevant” Evidence?
The VA defines “new and relevant evidence” under 38 CFR § 3.2501(a)(1) as:
- Information the VA has not previously reviewed.
Relevant:
- Evidence that tends to prove or disprove an element of your claim or
- Has a reasonable possibility of helping substantiate the claim.
In other words:
✔️ If the evidence strengthens any part of your case—and the VA didn’t have it before—it’s likely considered new and relevant.
This applies when filing a Supplemental Claim, which is the required lane for reopening denied claims under the AMA.
Why the “New and Relevant” Standard Matters
The VA won’t reconsider a denied claim unless the veteran submits evidence that clearly adds value. They won’t reevaluate the claim based on old statements, repeated arguments, or medical records already in the file.
But—this is important—the standard is intentionally lower than the previous “new and material” threshold, meaning veterans have a better chance of being reconsidered when the right evidence is submitted.

Examples of What DOES Count as New and Relevant Evidence
Below are real-world examples of evidence that typically meets the VA’s threshold.
1. A New Medical Diagnosis
If a veteran didn’t previously have a diagnosis—or it wasn’t clearly documented—a provider’s updated evaluation can completely shift the VA’s ruling.
Examples:
- First-time PTSD diagnosis
- Newly documented depression, anxiety, TBI, radiculopathy, sleep apnea, etc.
- Updated diagnosis showing condition has worsened
Why it matters:
A diagnosis is foundational. Without it, the VA cannot grant service connection.
2. A Nexus Letter Linking Your Condition to Service
One of the most powerful forms of new and relevant evidence a veteran can submit is a medical nexus letter—a professional medical opinion that explains how and why a current disability is connected to military service. When written correctly, a nexus letter can single-handedly reopen a denied claim and establish the missing link the VA needs to approve service connection.
A strong nexus letter must meet specific criteria to be accepted by the VA:
✔ Written by a Qualified Medical Professional
The provider should have the appropriate credentials, training, and clinical expertise to evaluate your specific condition. While the VA accepts opinions from both VA and private clinicians, the letter carries more weight when the provider:
- Understands VA disability standards
- Can speak to the medical science behind your condition
- Is familiar with how the VA evaluates service connection
Attain Med Group specializes in medical opinions tailored specifically to VA requirements, giving veterans the professional medical support needed to strengthen their claims.
✔ Based on a Thorough Review of Your Records
A nexus opinion is only credible if it’s grounded in a careful review of:
- Service Treatment Records (STRs)
- VA medical records
- Private medical records
- Prior C&P exam results
- Diagnostic tests, imaging, and lab reports
- Symptom timelines
- Incident or deployment records
This review allows the medical expert to connect the dots between in-service events and current symptoms—something the VA often fails to do in its initial evaluation.
✔ Supported by Clear Medical Reasoning and Evidence
A valid nexus letter cannot rely on vague statements such as “the veteran reports…” or “it is possible that…”
Instead, it must contain:
- Logical medical explanations
- Evidence-based analysis
- Clinical reasoning tying your symptoms to service events
- Citations from medical literature when appropriate
- A detailed rationale explaining how the medical conclusion was reached
This level of detail demonstrates credibility, expertise, and adherence to medical standards—key components of evidence the VA finds persuasive.
✔ Using the VA’s “At Least As Likely As Not” Standard
For the VA, the burden of proof is unique. The medical provider must state that the condition is: “at least as likely as not” (50% or greater probability) connected to service.
This is the legal threshold required for the VA to grant service connection. A statement of certainty (“definitely caused by”) is not required—only a medically supported probability of 50% or more.
Why Nexus Letters Matter
Most VA claim denials happen because the VA concludes the condition is “not service-connected” or “cannot be linked to military service.”
A well-written medical nexus letter directly addresses the most common reasons for denial by:
- Filling in gaps left by incomplete C&P exams
- Correcting inaccurate VA medical opinions
- Clarifying misunderstood or misinterpreted medical records
- Providing expert analysis on medical causation or aggravation
- Establishing secondary service connections
When the VA denies a claim due to lack of evidence, a clear, comprehensive nexus letter becomes the missing piece the VA needs to approve the claim.

3. A Medical Opinion Establishing a Secondary Service Connection
A secondary service connection medical opinion is one of the most impactful types of evidence a veteran can submit when reopening a claim or establishing a new disability. Instead of proving that the condition began in service, a secondary opinion shows that your existing, service-connected disability has caused—or aggravated—a new condition.
This approach is often far easier to prove and dramatically strengthens a claim when the direct service link is unclear or undocumented.
What Is a Secondary Service Connection?
Under 38 CFR § 3.310, a veteran may receive disability benefits for a condition that is:
- Caused by a service-connected disability, or
- Aggravated by a service-connected disability (worsened beyond natural progression).
A medical opinion must clearly state whether the condition is caused or aggravated and provide supporting medical reasoning. Without this distinction, the VA may reject or undervalue the evidence.
Examples of Valid Secondary Connections
Secondary connections are extremely common in the VA system—yet they are underutilized by many veterans because the relationships between conditions aren’t always obvious. High-quality medical opinions make these links unmistakably clear.
✔ Migraines Caused by PTSD
Medical research supports a strong correlation between PTSD and chronic migraines. Stress-response dysregulation, sleep disturbance, and hyperarousal can trigger persistent headaches. A medical opinion can explain this connection and tie your migraines directly to your service-connected PTSD.
✔ GERD Caused by Anxiety or Psychotropic Medications
Medications frequently prescribed for PTSD, anxiety, and depression—such as SSRIs, SNRIs, benzodiazepines, and NSAIDs—can significantly worsen acid reflux. A provider can demonstrate the pharmacological link between your treatment and your GERD symptoms.
✔ Radiculopathy from a Service-Connected Spine Condition
If you are already service-connected for a lumbar or cervical spine disability, nerve compression may develop later and radiate pain into the legs or arms. A medical opinion can show how degenerative disc disease or spinal arthritis led to new neurological deficits.
✔ Depression Secondary to Chronic Pain
Chronic musculoskeletal pain is a leading medical cause of depression. When a service-connected physical condition disrupts sleep, mobility, or daily functioning, it can significantly affect mental health. A clinician can connect the emotional toll of chronic pain to a secondary depressive disorder.

Why Secondary Opinions Matter
Secondary service connections are one of the most overlooked strategies for increasing ratings, reopening claims, or receiving compensation for conditions not formally documented during service. Many veterans suffer from downstream health problems caused by their primary disabilities, but the VA rarely recognizes these links without clear medical evidence.
A strong medical opinion:
- Expands the scope of your benefits
- Ensures the VA accounts for the full impact of your disabilities
- Helps overcome missing service records or undocumented in-service events
- Fills in medical gaps that C&P exams often miss
- Supports rating increases when symptoms worsen over time
For denied claims, secondary opinions often qualify as new and relevant evidence because they introduce a medically supported theory the VA did not previously consider.
4. New Treatment Records the VA Hasn’t Reviewed
Another powerful form of new and relevant evidence is any updated medical documentation that the VA did not consider during the original decision. Many veterans assume the VA automatically gathers all of their records—but this is rarely the case. If important medical reports were missing during your first review, providing them now can completely change the outcome of your claim.
What Types of Treatment Records Count?
Any medical documentation created after the initial decision—or records the VA failed to obtain before—can qualify as new and relevant evidence. These include:
✔ VA Medical Records
Many denied claims occur simply because the VA did not look at the most recent clinical notes or specialty evaluations in your VA health system. Updated documentation can clarify:
- Diagnosis changes
- Worsening symptoms
- New referrals or specialist findings
- Ongoing treatment plans
Even routine progress notes help establish chronicity over time.
✔ Private Physician Records
The VA does not automatically obtain private records. If you saw:
- A primary care physician
- Orthopedic or neurological specialist
- Cardiologist, gastroenterologist, or psychiatrist
- Any clinician outside the VA
…those records could be critical in proving service connection or severity.
Private records often contain more detailed evaluations, stronger diagnostic language, and clearer medical reasoning than VA notes—making them especially valuable.
✔ Therapy or Psychiatric Notes
For mental health claims, psychotherapy notes, medication management visits, and counseling summaries can provide:
- Symptom timelines
- Behavioral changes
- Severity descriptions
- Functional impairment documentation
- Support for both primary and secondary mental health connections
These records are essential for building a strong claim for depression, anxiety, PTSD, or related disorders.

✔ Urgent Care and Emergency Room Visits
Many vets seek urgent treatment during flare-ups. These episodes are incredibly important because they can document:
- Acute symptoms
- Functional limitations
- Incapacitating episodes
- Pain severity spikes
These records often reveal the true day-to-day impact of a disability better than scheduled appointments.
✔ Specialist Evaluations and Diagnostic Tests
New evaluations from specialists—such as gastroenterologists, rheumatologists, neurologists, ENTs, or pain management providers—carry significant weight, especially when they include:
- Confirmed diagnoses
- Imaging or lab findings
- Functional impairment assessments
- Medication side effects
- Expert medical interpretations
These insights can directly support service connection, secondary connection, or rating increases.
Why These Records Matter
Updated treatment records serve two critical purposes in the VA disability evaluation process:
1. They Prove Chronicity
The VA needs evidence that your condition is ongoing, not temporary. Consistent treatment notes demonstrate:
- Long-term symptoms
- Continuing medical need
- Patterns of flare-ups
- Persistent functional limitations
This directly supports service connection and rating increases.
2. They Demonstrate Severity
The frequency and intensity of medical visits help establish the true impact of your condition. Regular treatment indicates that symptoms significantly affect your health, daily functioning, and overall quality of life.
The VA heavily weighs:
- Specialist involvement
- Changes in medication
- Escalating treatment
- Repeated episodes of acute care
These indicators can shift a low rating to a higher one—or transform a denial into an approval.
3. New Evidence Showing Your Condition Has Worsened
When filing for a higher VA rating or reopening a denied claim, evidence that your condition has worsened can be one of the most impactful forms of new and relevant documentation. The VA must reconsider your claim if you provide proof that your symptoms, functional limitations, or medical needs have increased since the last evaluation.
This type of evidence is essential because the VA’s disability ratings are based on current severity—not past severity. If your condition has progressed, new documentation can justify a reevaluation and a higher compensable rating.

Types of Worsening Evidence the VA Accepts
Not all worsening is documented through imaging or lab tests. The VA accepts many forms of clinical and functional evidence showing that your disability now affects you more severely.
Below are examples that strongly support a claim.
✔ Updated Symptom Logs or Daily Journals
Tracking symptoms over time can demonstrate patterns of:
- Pain flare-ups
- Sleep disturbances
- Panic attacks
- Mobility limitations
- Migraines
- Gastrointestinal episodes
Daily logs provide real-world evidence of frequency, duration, and intensity—data the VA often fails to capture during short C&P exams.
✔ New Prescriptions or Increased Medication Dosages
If your provider has:
- Increased your dosage
- Added new medications
- Switched you to stronger treatments
- Recommended injections or procedures
…these are clear indicators that your condition is not controlled and may be worsening.
Medication changes are some of the most persuasive pieces of evidence the VA considers.
✔ Worsening Mental Health Symptoms
For depression, anxiety, PTSD, or other psychiatric diagnoses, worsening may show up through:
- Increased irritability or social withdrawal
- More frequent panic attacks
- Declining ability to function at work
- Reduced personal hygiene
- Heightened suicidal ideation
- Aggravation due to chronic pain or physical conditions
Therapists’ notes, psychiatry evaluations, and crisis-line contacts can all demonstrate significant deterioration.
✔ Employer or Supervisor Statements
Workplace documentation can be extremely valuable, especially for increased-rating claims. Useful statements may describe:
- Reduced productivity
- Difficulty following instructions
- More absences or tardiness
- Inability to perform physical tasks
- Decreased reliability or consistency
These statements show functional impairment—one of the primary rating factors for many VA disabilities.
✔ Recent Hospitalizations, ER Visits, or Urgent Care Treatment
Acute episodes resulting in emergency treatment carry significant weight because they indicate:
- Severe symptom spikes
- Incapacitating episodes
- Complications requiring immediate care
- Conditions that are unstable or deteriorating
Even one hospitalization can provide strong evidence for reevaluation.
Why Worsening Evidence Matters
Submitting new, credible documentation of worsening can:
- Trigger the VA’s duty to assist
- Strengthen rating increase requests
- Help overturn prior denials
- Provide clarity when C&P exams fail to capture severity
- Support both primary and secondary service connections
Because the VA bases decisions on the current level of impairment, showing a clear medical trend of deterioration is often the difference between a denied claim and a successful one.
4. Service Records the VA Never Reviewed
Sometimes the VA makes a decision without seeing all of the relevant service records. If important documents were missing from your file during the original review, you can submit them now to strengthen your claim. These records may contain critical evidence that directly links your condition to military service.
Examples of Service Records That May Have Been Overlooked
- Deployment Records
These can confirm where you were stationed, the conditions you were exposed to, or specific operations that may have contributed to your medical issues. - Training Accident Records
If you were injured during training exercises or field drills, these records provide direct documentation of the incident and any immediate medical treatment. - Line-of-Duty (LOD) Investigations
LOD findings can establish that an injury or illness happened during active service and wasn’t due to misconduct—making it compensable. - Incident / Accident Reports
These reports document specific events such as vehicle crashes, equipment malfunctions, exposures, or on-base injuries that could have led to your condition. - MOS-Related Duty Logs
Your military occupational specialty (MOS) may expose you to certain hazards—heavy lifting, repetitive motions, chemicals, combat stressors. Duty logs help connect your physical or mental health condition to daily responsibilities.

Why This Matters
When the VA never reviewed certain service records—especially ones that clearly support your claim—it means the previous decision may have been incomplete or incorrect.
These records are highly relevant because they can:
- Strengthen the direct connection between your condition and military service (nexus)
- Provide documented proof of in-service events, exposures, or trauma
- Clarify timelines that support continuity of symptoms
- Correct errors or missing information in the original VA decision
In short: If the VA didn’t have all the facts, you now have the opportunity to supply them—and potentially overturn or increase your rating.
7. Lay Statements the VA Never Considered
From:
- You
- Family members
- Spouses
- Employers
- Fellow service members (“buddy statements”)
Topics can include:
- When symptoms started
- How symptoms affect daily life
- Observable physical or mental health changes
8. Independent Medical Exams (IMEs) or Disability Benefits Questionnaires (DBQs)
Especially when completed by specialists familiar with VA standards.
Why it matters:
DBQs provide structured, VA-compliant documentation that can fill gaps the VA exam left.
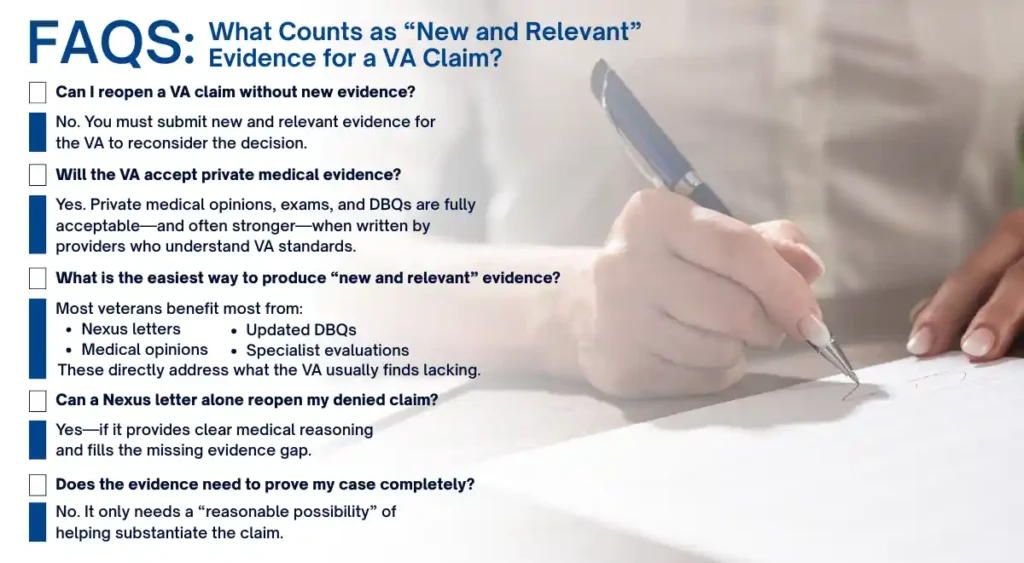
What Does NOT Count as “New and Relevant” Evidence?
The VA rejects evidence that:
✘ Is already in your file
Submitting duplicates does nothing.
✘ Repeats the same statements without new details
Simply saying “I disagree with the decision” is not evidence.
✘ Doesn’t connect to your claim
Evidence must strengthen at least one missing component:
- Diagnosis
- Nexus
- Severity
- Service connection
✘ Is vague, incomplete, or medically unsupported
For example:
- Unsupported nexus letters
- One-line doctor opinions
- Notes with no reasoning or rationale
✘ Contains no professional medical input when needed
Mental health, sleep apnea, migraines, and musculoskeletal conditions almost always require expert medical evidence—not just lay statements.
Why Many Veterans Get Denied: The “Evidence Gap” Problem
Most VA denials happen because ONE of the required pillars is missing:
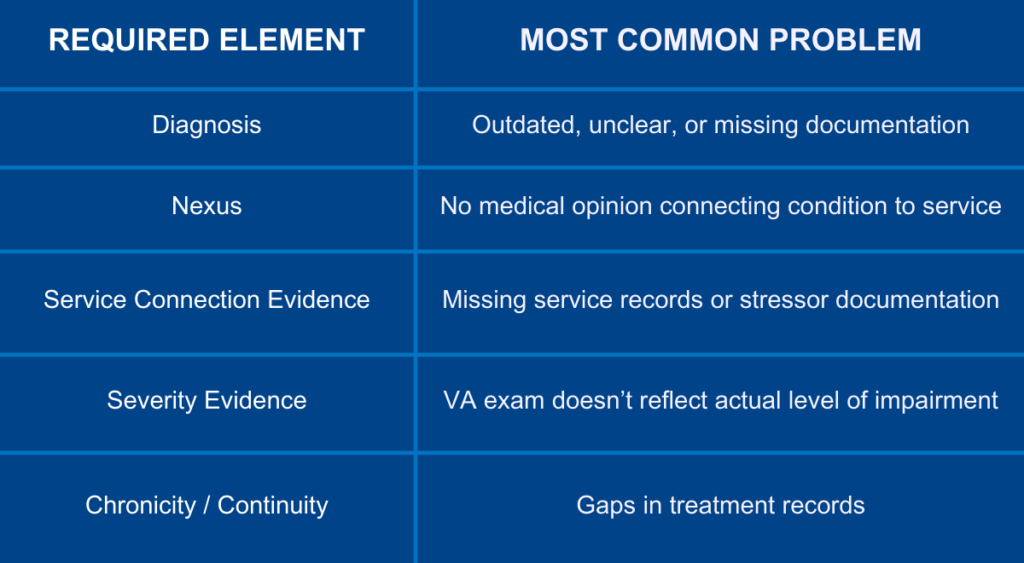
Attain Med Group exists to fill these evidence gaps with expert-prepared medical documentation that directly satisfies VA requirements.
How Medical Opinions Can Reopen Denied Claims
When the VA denies a claim, it’s often because the evidence in the file didn’t clearly connect your condition to your service—or didn’t show how severe your symptoms truly are. This is where new medical opinions become extremely powerful.
Medical evidence is one of the strongest forms of “new and relevant” evidence the VA recognizes. The right medical documents can directly challenge the VA’s prior conclusions, fill in gaps, and provide the missing explanation the VA needs to approve your claim.

Types of Medical Evidence That Can Reopen a Denied Claim
✔ Nexus Letters
A well-written nexus letter explains the medical link between your current condition and an in-service event, injury, exposure, or another service-connected disability. It provides the “because of” or “at least as likely as not” explanation that the VA often says was missing.
✔ Secondary Connection Opinions
These opinions show how a service-connected condition caused or aggravated a new condition. Example: PTSD leading to sleep apnea, GERD, migraines, or hypertension. Secondary opinions open up claims that were previously denied due to lack of medical reasoning.
✔ Independent Medical Exams (IMEs)
An IME provides an unbiased, third-party medical assessment that can challenge a flawed VA C&P exam. If the previous VA examiner missed symptoms or made inaccurate conclusions, an IME can correct the record.
✔ Disability Benefits Questionnaires (DBQs) With Strong Rationale
A DBQ that includes detailed explanations—not just checked boxes—is far more persuasive. When the doctor explains how and why your symptoms meet a higher severity level, the VA is required to consider it.
✔ Symptom Progression Reviews
These reviews document how your condition has worsened over time. Progression evidence can support an increased rating, especially when symptoms have escalated since your last VA decision.
✔ Medical Records Analyses
A physician-expert can review your past service records, medical records, and denial letters to highlight errors, overlooked events, or misinterpreted findings. This type of expert interpretation adds clarity the VA may have missed.

Why These Medical Opinions Matter
When done professionally, these medical documents provide the VA with the exact type of evidence needed to overturn a denial. They can:
✔ Address VA Errors
If the VA misinterpreted or ignored evidence, a medical opinion can directly point out and correct those mistakes.
✔ Correct Inaccurate VA Exams
C&P examiners sometimes rush or overlook key symptoms. A strong independent medical opinion can offer a more accurate assessment of your condition.
✔ Provide Missing Rationale
Many denials happen because the VA says the evidence “lacked rationale.” Medical opinions fill in the missing explanation with clear, authoritative medical reasoning.
✔ Demonstrate Chronicity or Aggravation
Doctors can show that your condition has been ongoing, worsening, or aggravated by another service-connected issue—which is crucial for both service connection and rating increases.
✔ Strengthen Credibility and Medical Accuracy
When evidence is logically structured, medically sound, and supported by records, it significantly increases the strength of your overall claim.

Step-by-Step: How to Reopen Your Claim with New and Relevant Evidence
Reopening a VA claim can feel complex, but following a structured approach ensures you submit the strongest possible evidence. Below is a step-by-step roadmap to guide veterans through the process.
1. Request Your VA C-File
Before submitting new evidence, it’s critical to review what the VA already has on file. Your C-File (claims file) contains all records, medical opinions, and prior VA decisions related to your claim.
Why this matters:
- Prevents submitting duplicate information
- Helps identify gaps or missing documentation
- Allows you to focus on what counts as new and relevant evidence
You can request your C-File directly from the VA or use a third-party service to ensure you receive a complete copy.
2. Identify the Reason for Denial
Carefully read the VA decision letter to determine why your claim was denied. Common reasons include:
- Insufficient evidence – The VA didn’t see enough proof of your condition or its link to service
- No nexus – The connection between your condition and service wasn’t established
- Condition not related to service – The VA concluded your disability was unrelated to military service
Understanding the denial reason is crucial to know what type of new evidence will make a difference.
3. Determine the Missing Evidence Type
Once you know why your claim was denied, identify the exact type of evidence needed to strengthen your case. This may include:
- Diagnosis – Medical documentation confirming your condition exists
- Nexus – A medical opinion linking your condition to service
- Severity evidence – Records or logs showing how the condition impacts daily life
- Treatment history – VA or private records that show chronicity or worsening symptoms
Pinpointing the gap ensures you submit evidence the VA will consider relevant.
4. Collect or Update Your Medical Records
Gather all relevant medical documentation, ensuring it is:
- Current – Recent treatment notes, hospital visits, or specialist evaluations
- Detailed – Include symptom severity, functional limitations, and impact on daily life
- Comprehensive – Cover both primary conditions and potential secondary connections
Private medical records, VA treatment notes, and specialist evaluations are all valuable.
5. Obtain an Expert Medical Opinion or Nexus Letter
This step is often the most critical for reopening a denied claim. A qualified medical professional can:
- Clearly explain how your condition is connected to service
- Provide expert reasoning supporting secondary service connections
- Demonstrate chronicity, progression, or aggravation of your disability
- Write the opinion according to the VA’s “at least as likely as not” standard
Expert opinions bridge gaps that your medical records alone may not cover, giving your claim a strong, credible foundation.
6. Submit a Supplemental Claim (VA Form 20-0995)
Once all new evidence is gathered, file a Supplemental Claim using VA Form 20-0995.
Tips for submission:
- Include all new and relevant medical evidence
- Clearly reference each document in your cover letter
- Highlight how this evidence addresses the denial reason
- Keep copies of everything submitted
The supplemental claim process is specifically designed to allow veterans to reopen denied claims with new and relevant evidence.
7. Track Your Claim Through VA.gov
After submission:
- Monitor the status of your claim online.
- Respond promptly to VA requests for additional information
- Keep detailed records of all communications and submissions
Tracking ensures you remain proactive and can address any follow-up questions quickly.

Bottom Line
Reopening a VA claim isn’t just about submitting more paperwork—it’s about submitting targeted, new, and relevant evidence that fills gaps the VA previously identified. By systematically reviewing your file, identifying what’s missing, and leveraging professional medical opinions, you maximize your chances of approval or rating increases.
Strengthen Your Supplemental Claim with Expert Medical Evidence
If your claim was denied—or you’re trying to reopen a previously denied condition—you don’t have to navigate VA evidence requirements alone.
Attain Med Group is the most trusted name in medical evidence for VA disability claims because we provide:
- ✔ Expert Nexus Letters
- ✔ Independent Medical Opinions
- ✔ VA-compliant DBQs
- ✔ Detailed medical records reviews
- ✔ Clear, defensible medical rationale
- ✔ Veteran-centered support every step of the way
Our mission is simple:
Provide the medical evidence veterans need to secure the benefits they’ve earned. Ready to Reopen Your Claim? Start With a Free Case Review.
If your claim was denied due to lack of evidence—or you’re unsure what qualifies as new and relevant—our team is here to help.
👉 Contact Attain Med Group today to get expert medical support tailored to your VA disability claim.