Depression and anxiety are among the most misunderstood—and most frequently underrated—VA disability claims. Many veterans assume that simply having a diagnosis is enough. In reality, the VA requires specific types of medical evidence, detailed functional documentation, and a clear link between your mental health symptoms and your service.
As a veteran-owned, veteran-centered organization, Attain Med Group specializes in providing the medical expertise, nexus opinions, DBQs, and clinical documentation veterans need to secure the ratings they deserve. This guide breaks down exactly what evidence the VA accepts—and how to build a strong, fully supported mental health claim.
Why Mental Health Claims Are Commonly Denied or Underrated
Despite being some of the most widespread conditions among veterans, depression and anxiety claims often fail because:
- Veterans submit only a diagnosis, with no supporting medical rationale
- Symptoms are downplayed or not consistently documented
- The C&P exam does not reflect real functional limitations
- No nexus letter connects symptoms to military service
- Stressor events are unclear, undocumented, or challenged by the VA
To win your claim—and to secure an accurate rating—you must understand the exact evidence the VA evaluates.
How the VA Rates Depression and Anxiety
The VA uses the same rating schedule (38 CFR § 4.130) for most mental health conditions, including:
- Major depressive disorder
- Generalized anxiety disorder
- Adjustment disorder
- Panic disorder
- PTSD
- OCD
- Other trauma-related disorders
Ratings range from 0% to 100%, based on functional impairment, not just diagnosis or symptom list.
VA Mental Health Rating Factors
When evaluating depression, anxiety, or any service-connected mental health condition, the VA does not base the rating solely on the diagnosis. Instead, the VA looks at how your symptoms impact your daily life, using four core rating factors. Understanding these factors is critical for building strong medical evidence that matches what VA raters are trained to evaluate.
1. Occupational Impairment is one of the most influential elements in determining your mental health rating. The VA wants to understand how your symptoms affect your ability to:
- Obtain employment
- Maintain steady work
- Perform job duties consistently and reliably
Examples of occupational challenges the VA may consider:
- Difficulty keeping a job due to emotional instability, panic, or frequent absences
- Reduced reliability or productivity, such as struggling to complete tasks or maintain focus
- Problems concentrating or following instructions, especially in high-stress or fast-paced environments
- Interpersonal conflicts, including arguments with coworkers, supervisors, or customers
- Difficulty adapting to workplace stress, which is specifically cited in higher VA rating levels
- Needing to work alone or in reduced-stimulation environments because of anxiety, irritability, or panic
The more your symptoms interfere with your ability to function in a work setting, the more likely the VA is to assign a 50%, 70%, or even 100% rating.
2. Social Impairment. The VA also evaluates how your mental health condition affects your ability to interact with others and maintain healthy relationships.
Social impairment can include:
- Isolation or withdrawal from family, friends, or social activities
- Irritability or anger, leading to strained personal interactions
- Marital or relationship strain, including communication problems or emotional disconnection
- Difficulty trusting others, especially common in trauma-related conditions
- Loss of interest in hobbies or activities you once enjoyed
- Avoidance of crowds, gatherings, or public places due to anxiety
- Feeling detached or emotionally numb
These social challenges help the VA determine whether symptoms are mild, moderate, or severe—and whether they affect overall functioning enough to qualify for higher ratings.

3. Frequency, Duration, and Severity of Symptoms
One of the most important rating factors is how often symptoms occur (frequency), how long episodes last (duration), and how disabling they are (severity). The VA evaluates patterns, consistency, and the overall impact on daily life.
Common symptoms the VA weighs heavily include:
- Panic attacks, especially those occurring more than once a week (a criterion for the 50% rating level)
- Depressed mood that makes routine activities difficult
- Chronic sleep impairment, which affects daytime functioning, mood, focus, and energy
- Memory or concentration problems, from mild forgetfulness to serious cognitive impairment
- Suicidal ideation, which can qualify a veteran for a 70% rating even when other symptoms are moderate
- Impaired judgment, including impulsive decisions, emotional outbursts, or poor risk assessment
- Difficulty adapting to stressful circumstances, including work environments, changes in routine, or family conflict
The VA looks for patterns over time, not isolated incidents—this is why ongoing medical documentation is crucial.
4. Medical Evidence Supporting the Diagnosis. A diagnosis by itself does not guarantee a rating. The VA requires credible, consistent, and well-documented medical evidence to support your claim.
This includes:
- Clinical treatment records from mental health providers
- Medication history, including antidepressants, anti-anxiety medications, sleep aids, or mood stabilizers
- Therapy notes, showing ongoing symptoms, progress, or setbacks
- Psychological evaluations or neuropsychological testing
- Independent medical opinions or nexus letters, especially when connecting your condition to service
- DBQs (Disability Benefits Questionnaires) completed by qualified clinicians
- Hospitalization records, if applicable
- Crisis intervention or emergency room visits related to mental health
VA raters are trained to look for consistency over time. If your records show repeated mentions of panic attacks, sleep disturbance, depression, or social withdrawal, it strengthens your claim significantly.
What Evidence the VA Actually Accepts for Depression and Anxiety
To win your mental health claim, you need to provide specific categories of evidence demonstrating severity, functional impact, and service connection.
Below is what the VA considers credible and compelling.
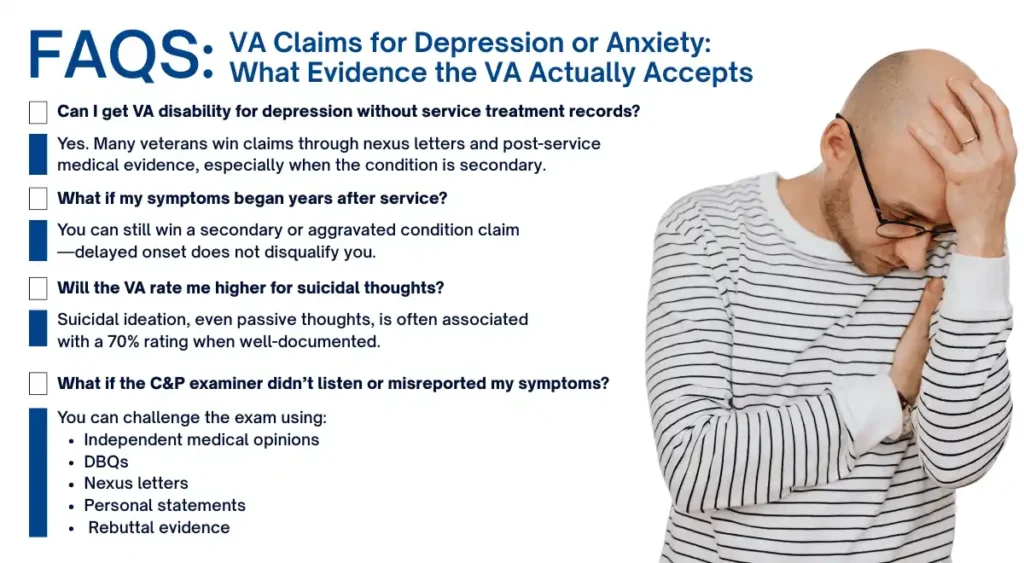
1. A Clear, Current Diagnosis from a Qualified Provider
The VA requires a mental health diagnosis from:
- A psychologist (PhD/PsyD)
- A psychiatrist (MD/DO)
- A licensed clinical mental health provider
Self-reported symptoms alone are not enough.
Why this matters:
Mental health conditions can overlap. A precise diagnosis anchors your entire claim and determines how the VA evaluates your symptoms.
2. Medical Nexus Evidence Linking Depression or Anxiety to Service
This is the #1 missing piece in denied mental health claims.
A nexus letter from an independent medical provider can establish:
- Direct service connection
Example: symptoms began after a deployment, MST event, injury, or traumatic event - Secondary service connection
Example: depression or anxiety caused by chronic pain, tinnitus, GERD, migraines, or physical disability - Aggravation
Example: pre-existing anxiety worsened permanently due to military stressors
A strong nexus letter includes:
- A review of medical records
- Clinical rationale
- Peer-reviewed research references
- A “more likely than not” (or higher) medical opinion
- Documentation explaining the veteran’s symptom progression
Attain Med Group specializes in crafting medically sound, defensible nexus letters that directly address VA requirements.
3. Detailed Treatment Records and Clinical Notes
The VA looks for consistency. This includes:
- Ongoing therapy sessions
- Medication history
- Hospitalizations
- Mental health screenings
- Notes about mood, sleep, panic attacks, or social withdrawal
These records show the trajectory and severity of your condition over time.
4. Evidence of Functional Loss (What Matters Most to VA Raters)
The VA cares about how your mental health condition affects daily life, including:
Work-related functional loss
- Missing work
- Difficulty concentrating
- Inability to follow complex tasks
- Conflicts with coworkers or supervisors
Social functional loss
- Avoiding social situations
- Problems maintaining friendships
- Family relationship strain
- Emotional withdrawal
Daily-life functional loss
- Difficulty leaving the house
- Panic in public spaces
- Neglect of personal appearance or hygiene
- Disrupted sleep affecting daytime functioning
These functional impacts often determine whether a veteran receives a 30%, 50%, 70%, or 100% rating.
5. Lay Statements That Support Your Condition
The VA accepts statements from:
- Family members
- Spouses
- Friends
- Supervisors
- Coworkers
- Fellow service members
Lay statements should describe:
- Behavioral changes
- Emotional instability
- Specific events (e.g., panic attacks or breakdowns)
- Social isolation
- Decline in work performance
They help corroborate symptoms the VA cannot measure directly.

6. Strong Performance in the C&P Exam (and How to Prepare)
The Compensation & Pension (C&P) exam heavily influences your rating.
To prepare:
- Describe your worst days—not just your good days
- Be honest, specific, and consistent
- Explain how symptoms affect work, relationships, and daily functioning
- Avoid minimizing symptoms
- Provide examples (panic attacks, isolation, sleep issues, etc.)
Your aim is clarity, not exaggeration.
7. Independent Medical Opinions and DBQs
A Disability Benefits Questionnaire (DBQ) from an experienced mental health clinician can:
- Document symptoms in VA-accepted language
- Strengthen your functional impairment evidence
- Provide a medical foundation for rating levels
- Correct errors from a poor C&P exam
Attain Med Group’s network of independent medical providers is trained specifically in VA-compliant documentation, ensuring your evidence meets VA standards.

Conditions Often Secondary to Depression or Anxiety
Veterans frequently qualify for additional ratings for conditions caused by or aggravated by depression or anxiety, such as:
- Insomnia
- Headaches or migraines
- IBS or GERD
- Chronic pain disorders
- Hypertension
- Sexual dysfunction
- Substance use disorder
- Weight gain or loss
- Cognitive or memory impairment
Secondary claims can significantly increase your combined rating.
Example: What a Strong Mental Health Claim Looks Like
A successful claim typically includes:
- Diagnosis from a licensed mental health professional
- Consistent treatment and medication records
- Detailed symptom descriptions
- Nexus letter linking condition to service
- DBQ documenting occupational and social impairment
- Lay statements supporting long-term symptoms
- Accurate, honest C&P exam responses
This is the level of documentation that Attain Med Group prepares for veterans every day.
Final Thoughts: You Don’t Have to Face Mental Health Claims Alone
VA mental health claims require far more than a diagnosis—they demand structured, medically sound evidence and expert documentation. With the right support, veterans can secure strong, accurate ratings that reflect the true impact of their condition.
Attain Med Group is the nation’s most trusted provider of medical evidence for VA disability claims. As a veteran-owned and veteran-centered team, we specialize in:
- Independent medical nexus letters
- Mental health DBQs
- Medical record reviews
- Condition-specific evaluations
- Expert documentation built for VA standards

Get the Medical Evidence You Need to Win Your Claim
Your story deserves to be heard—and your symptoms deserve to be taken seriously.
👉 Book a consultation with Attain Med Group today and take the next step toward the benefits you’ve earned.