Traumatic Brain Injury (TBI) can change a veteran’s life in ways that aren’t always obvious. When seeking VA disability benefits, these hidden effects of TBI often create challenges during the evaluation process. This gap in understanding can leave many disabled veterans without the full disability compensation they need and deserve for their health condition.
Traumatic brain injuries are more common among veterans than many realize, often resulting from the unique exposures during military service. Combat situations involving explosions, vehicle accidents, falls during training, or direct head trauma can all lead to these brain injuries. Recognizing and thoroughly documenting how TBIs affect brain function and daily life is the core challenge for VA claims.
This article sheds light on the less visible consequences of TBI and their connection to VA disability ratings. We will explore why these impacts frequently go underrated in a TBI claim and what service members can do. The goal is to help veterans secure accurate recognition for their TBI within their disability claims.
What is Traumatic Brain Injury (TBI)?
A TBI happens when a sudden, external physical force disrupts the normal brain function. For veterans, common causes include blast waves from IEDs, impacts during combat, vehicle rollovers, parachute mishaps, or even falls during routine duties. The severity of a traumatic brain injury can vary widely, affecting individuals differently.
TBIs are categorized by severity: mild, moderate, and severe TBI. A mild traumatic brain injury (mild TBI), sometimes called a concussion, might involve a brief loss of consciousness or feeling dazed. Moderate and severe TBI involve longer periods of unconsciousness, memory loss, or penetrating head trauma, often leading to more significant long-term issues.
The effects of TBI aren’t always immediate or purely physical; they can manifest over time and impact cognitive abilities, emotional regulation, and behavior. Understanding the nature of TBI is the first step in recognizing its potential long-term impact on veterans disability and the need for appropriate health care.
The Hidden Symptoms of TBI
While some TBI symptoms like loss of consciousness are immediate, many TBI residual effects emerge gradually or are less obvious. These hidden symptoms significantly affect a veteran’s life but can be easily missed or misattributed during the claims process. It’s crucial to understand how TBIs affect brain function in diverse ways.
Cognitive impairment is common after TBI. This includes issues like persistent memory loss, difficulty concentrating or paying attention, slowed thinking, and problems with executive functions. Executive functions involve planning, organizing, problem-solving, and making decisions, which are vital for work and daily tasks.
Emotional impairments and behavioral changes are also frequent consequences. Veterans might experience increased irritability, mood swings, depression, anxiety, or personality changes that impact social interaction and relationships. These emotional impairments can be just as disabling as physical symptoms.
Physical symptoms often persist long after the initial head trauma. Chronic headaches or migraines, dizziness, balance problems, chronic fatigue, sleep disturbances like insomnia or sleep apnea, and heightened sensitivity to light or sound are common complaints. These physical issues compound the difficulties faced by veterans with TBI.
Why TBI Often Goes Underrated in VA Disability Claims
Several factors contribute to TBI being frequently underrated in VA disability claims, preventing veterans from receiving an accurate TBI disability rating. A primary reason is the overlap between TBI symptoms and other common veteran health conditions. Conditions like Post-Traumatic Stress Disorder (PTSD), depression, anxiety, or even chronic fatigue can present with similar symptoms, such as memory problems, irritability, and sleep disturbances.
This symptom overlap can lead evaluators to attribute problems solely to a mental health condition like a stress disorder, overlooking the contribution of the brain injury itself. It requires careful medical evaluation to differentiate and properly assess the impact of each condition. Getting the TBI diagnosis correct and linking it to service is vital.
Another challenge is the delayed onset of some TBI symptoms. Cognitive or emotional changes might not become apparent until months or years after the TBI exposure event during military service. This time gap can make establishing service connection more difficult, as the link between the initial injury and current symptoms seems less direct without strong medical evidence and potentially a nexus letter.
Furthermore, awareness and understanding of the full spectrum of TBI symptoms, especially those associated with mild traumatic brain injury, may be lacking among both veterans and some healthcare providers. Veterans might not realize certain difficulties stem from a past head trauma, or medical record documentation might be incomplete. This can result in an underdeveloped TBI claim submitted to the Veterans Affairs regional office.
The Impact of TBI on Daily Life
The consequences of TBI ripple through nearly every aspect of a veteran’s life, often in ways that aren’t immediately linked back to the initial brain injury. These daily struggles highlight why accurate disability ratings are so important for receiving adequate support and monthly compensation. The effects fundamentally alter how the brain function result impacts daily activities.
1. Work Performance and Employability
Cognitive impairment from TBI poses significant barriers to employment. Difficulties with memory loss, attention, concentration, and especially executive functions can make it challenging to learn new tasks, manage time effectively, or handle complex job responsibilities. Veterans may struggle to maintain consistent work performance, leading to job loss or underemployment, potentially necessitating a claim for total disability based on individual unemployability (TDIU).
Challenges with social interaction due to emotional impairments like irritability or mood swings can also affect workplace relationships. Maintaining professional conduct and teamwork might become difficult. These functional impacts are critical factors in determining the severity of the disability.
2. Relationships and Social Interaction
Personality changes, mood swings, irritability, and difficulty controlling impulses stemming from TBI can strain relationships with family, friends, and partners. Communication can become challenging, leading to misunderstandings and conflict. This can result in social isolation, further impacting mental health and overall well-being.
Veterans may withdraw from social activities due to sensory sensitivities (like noise or light) or cognitive fatigue. The impact on social interaction is a significant, though often overlooked, consequence that affects quality of life. Support systems can weaken just when they are needed most.
3. Physical Health and Secondary Conditions
The physical symptoms of TBI, such as chronic headaches, dizziness, and sleep disturbances, are debilitating on their own. Poor sleep, often linked to conditions like sleep apnea which has an increased risk after TBI, can worsen cognitive issues and contribute to chronic fatigue. This creates a cycle where physical symptoms exacerbate cognitive and emotional difficulties.
Furthermore, TBI can increase the risk of developing other serious health conditions later in life. These are known as secondary conditions and can include depression, anxiety, seizure disorders, Parkinsonism, and dementia. These secondary conditions add another layer of complexity to the veteran’s health care needs and disability claims process.
The Complexity of VA Disability Ratings for TBI
The Department of Veterans Affairs (VA) evaluates TBI under specific criteria outlined in the Code of Federal Regulations (CFR), Title 38, Part 4, using Diagnostic Code 8045. The VA rates TBI based on the residual effects of the injury, grouped into three main categories of dysfunction. These categories are cognitive, emotional/behavioral, and physical.
The VA evaluates the level of impairment in each category separately using a standardized table. This table assesses functions like memory, attention, concentration, executive functions (cognitive); depression, anxiety, irritability (emotional/behavioral); and subjective physical symptoms. The overall TBI disability rating is determined by the highest level of impairment found in any single category, not by combining scores from different categories.
The possible VA disability ratings for TBI residuals are 0%, 10%, 40%, 70%, or 100%. A 100% rating reflects total impairment in one or more areas, while lower ratings reflect varying degrees of difficulty. Achieving the highest disability rating generally requires profound cognitive impairment or severe disruption in work, social settings, or self-care due to emotional or behavioral issues.
Here is a simplified overview of how TBI residuals might be evaluated for a VA rating:
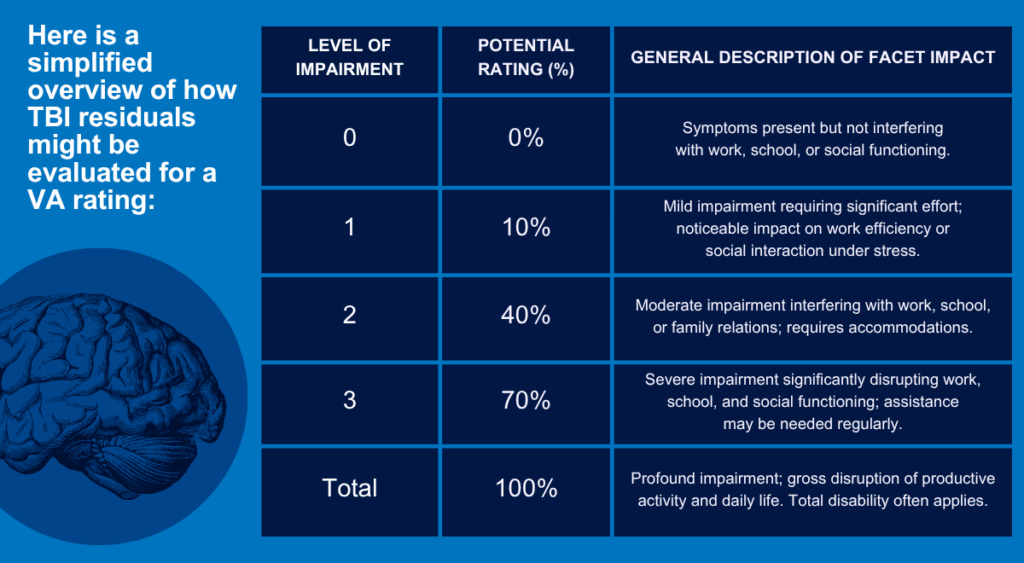
This system aims to capture the multifaceted nature of how TBIs affect brain function. However, accurately assessing and documenting the severity across these areas can be challenging, contributing to potential underrating if evidence is insufficient. Special Monthly Compensation (SMC) might be awarded in cases of particularly severe TBI requiring aid and attendance, representing additional monthly compensation beyond the standard va rates.
Why Comprehensive Medical Evidence is Crucial
Obtaining a fair VA disability rating for TBI hinges on providing thorough and relevant medical evidence. This evidence must establish the TBI diagnosis, link it to military service (service connection), and clearly demonstrate the current level of functional impairment. Simply having a TBI diagnosis in your medical record is often not enough.
1. Detailed Neuropsychological Evaluations
Neuropsychological testing is often vital for TBI claims. These specialized tests objectively measure cognitive functions like memory, attention, processing speed, and executive functions. The results provide concrete data on cognitive impairment that might not be obvious during routine medical appointments, offering strong support for the disability claim.
2. Comprehensive Nexus Letters
A nexus letter from a qualified medical professional is extremely valuable, especially if the TBI wasn’t diagnosed during service or if symptoms had a delayed onset. This letter explicitly connects the veteran’s current TBI residuals to the specific event or injury during military service. A strong nexus letter analyzes the veteran’s medical history, TBI exposure, current symptoms, and provides a medical opinion linking them based on available evidence.
3. Complete Medical Records
Gathering all relevant medical records is fundamental. This includes Service Treatment Records (STRs), VA medical records, and records from any private health care providers. These documents should ideally contain information about the initial head trauma, ongoing treatment, documented symptoms (headaches, memory loss, etc.), and any formal TBI diagnosis.
4. Buddy Statements and Personal Journals
Statements from fellow service members who witnessed the TBI event or observed subsequent changes in the veteran can provide crucial context, particularly if medical records are sparse. A personal journal detailing daily symptoms, challenges with work or social interaction, and the overall impact on life can also serve as compelling evidence. This helps illustrate the real-world effects of the TBI residual issues.
Secondary Conditions Linked to TBI
It’s important for veterans with TBI to understand the concept of secondary conditions. These are health conditions that develop as a result of, or are significantly worsened by, a service-connected disability. TBI is known to have an increased risk factor for several other health problems.
Common secondary conditions linked to TBI include mental health conditions such as depression, anxiety, and even PTSD (though PTSD can also be co-occurring). Sleep apnea is another frequently associated condition, possibly due to TBI affecting the brain’s regulation of breathing during sleep. Chronic headaches or migraines, seizure disorders, Parkinsonism, and cognitive impairment consistent with early dementia are other potential long-term consequences.
Veterans can file VA claims for these secondary conditions. If the VA agrees that the secondary condition is medically linked to the service-connected TBI, it can be granted service connection on a secondary basis. This can lead to an increased overall disability rating and higher monthly compensation, reflecting the broader health impact of the initial brain injury.
The Role of Specialized Medical Documentation
Navigating the VA claims process for TBI can be difficult due to the specific documentation requirements. Some organizations and medical professionals specialize in evaluating veterans and preparing detailed medical documentation tailored to VA standards. Their understanding of TBI, VA rating criteria (like VA rates TBI), and the importance of demonstrating functional impact can be beneficial.
These specialists focus on conducting thorough evaluations, including potentially necessary neuropsychological testing, and writing comprehensive reports or nexus letters. They aim to capture the full extent of the TBI residual symptoms and their effects on daily living, work, and social interaction. Quality medical evidence strengthens disability claims.
Working with professionals experienced in TBI and VA disability claims can help ensure that subtle but significant symptoms are properly documented. This meticulous approach helps build a stronger case for an accurate TBI disability rating. Remember, thorough documentation is key to validating your experience.
Steps Veterans Can Take to Improve Their TBI Disability Claims
If you are a veteran pursuing a TBI disability claim, proactive steps can strengthen your case. Preparing thoroughly increases the chances of receiving an appropriate disability rating and the corresponding disability benefits. Here’s how you can approach the VA claims process:
- Keep a detailed symptom journal: Document your daily symptoms (cognitive, emotional, physical), noting their frequency, severity, and impact on your activities, work, and relationships. This personal record provides valuable insight beyond clinical notes.
- Seek regular medical care and follow-up: Consistently attend appointments with VA health care providers or private physicians. Report all symptoms honestly and ensure they are documented in your medical record. Follow through with recommended treatments or therapies.
- Consider obtaining independent medical evidence: If feasible, getting an Independent Medical Examination (IME) or neuropsychological testing from a private specialist experienced with TBI can provide crucial objective evidence. A strong nexus letter can also be obtained this way.
- Work with accredited representation: Veterans Service Organizations (VSOs), accredited claims agents, or attorneys specializing in veterans disability law can provide invaluable assistance. They understand the claims process, evidence requirements, and how to present your case effectively to the regional office.
- Gather supporting statements: Request “buddy statements” from individuals who served with you and witnessed the TBI event or noticed changes afterward. Statements from family or friends describing your current struggles can also be helpful.
- Understand the C&P exam: Prepare for your Compensation & Pension (C&P) exam by reviewing your symptoms and records. Be honest and detailed with the examiner about how TBI affects your daily life and brain function.
- Don’t hesitate to appeal: If you receive an unfavorable decision or believe your TBI disability rating is too low, you have the right to appeal. An accredited representative can guide you through the appeals process for your VA claim.
- Explore other benefits: Depending on the severity of your TBI and its impact on your ability to work, consider looking into Social Security Disability Insurance (SSDI) as well. Meeting the criteria for Social Security disability can sometimes support a claim for TDIU with the VA.
Taking these steps demonstrates diligence and helps build a comprehensive picture of your condition for the Veterans Affairs adjudicators. Remember, this process is about accurately reflecting the challenges you face due to your service-connected TBI.
The Importance of Ongoing Care and Support
Receiving a VA disability rating and compensation for TBI is an important step, but managing the condition is an ongoing process. TBI often requires long-term management strategies and support systems. Consistent health care is vital for optimizing quality of life.
Various therapies can help manage TBI residual effects. Cognitive rehabilitation therapy can teach strategies to cope with memory loss and attention problems. Occupational therapy helps adapt daily tasks, while physical therapy can address balance issues or dizziness.
Mental health support is also crucial, given the high rates of depression, anxiety, and emotional impairments associated with TBI. Counseling, therapy, and sometimes medication can help manage mood swings, irritability, and other emotional challenges. Connecting with support groups for TBI survivors can provide peer understanding and coping strategies.
The VA offers specialized programs and resources for veterans dealing with traumatic brain injuries through its Polytrauma System of Care. These services range from inpatient rehabilitation for severe TBI to outpatient clinics offering comprehensive care plans. Utilizing these VA resources is important for long-term well-being and managing your health condition effectively.
Conclusion
The hidden impact of Traumatic Brain Injury often complicates the path to securing fair VA disability ratings. Many veterans find their TBI residuals, particularly subtle cognitive impairment or emotional impairments, are overlooked or underestimated in the disability claims process. Achieving proper recognition requires understanding the full spectrum of symptoms and how TBIs affect brain function long after the initial head trauma.
Successfully navigating the VA system depends heavily on comprehensive medical evidence, including detailed evaluations, consistent medical records, and potentially strong nexus letters linking symptoms to military service TBI exposure. Recognizing the potential for secondary conditions like sleep apnea or mental health conditions, and claiming them appropriately, is also vital for obtaining full disability benefits reflecting the true impact of the brain injury.
You served your country, and you deserve support for the injuries sustained during that service. By diligently documenting symptoms, seeking appropriate medical care, understanding the VA rates TBI process, and potentially seeking help from experienced representatives, veterans can improve their chances of receiving an accurate TBI disability rating and the monthly compensation needed. Don’t let the invisible wounds of TBI prevent you from getting the veterans disability support you have earned.